Constipation is a common issue in inpatient settings for different reasons (Medications side effects, lack of ambulation, change in meal habits and types, electrolyte disturbances, and dehydration).
Asking our patients about bowel movements is one of my daily rounding checklists.
The five-step approach to minimize constipation in hospitalized patients
- Ambulation
- Adequate hydration.
- Correct any electrolyte disturbances.
- Prescribe a scheduled bulking agent or a stool softener unless the patient has diarrhea.
- Prescribe as needed osmotic or stimulant laxatives.
For patients on home laxatives, we continue them as long as they are not presenting with diarrhea.
Laxatives types
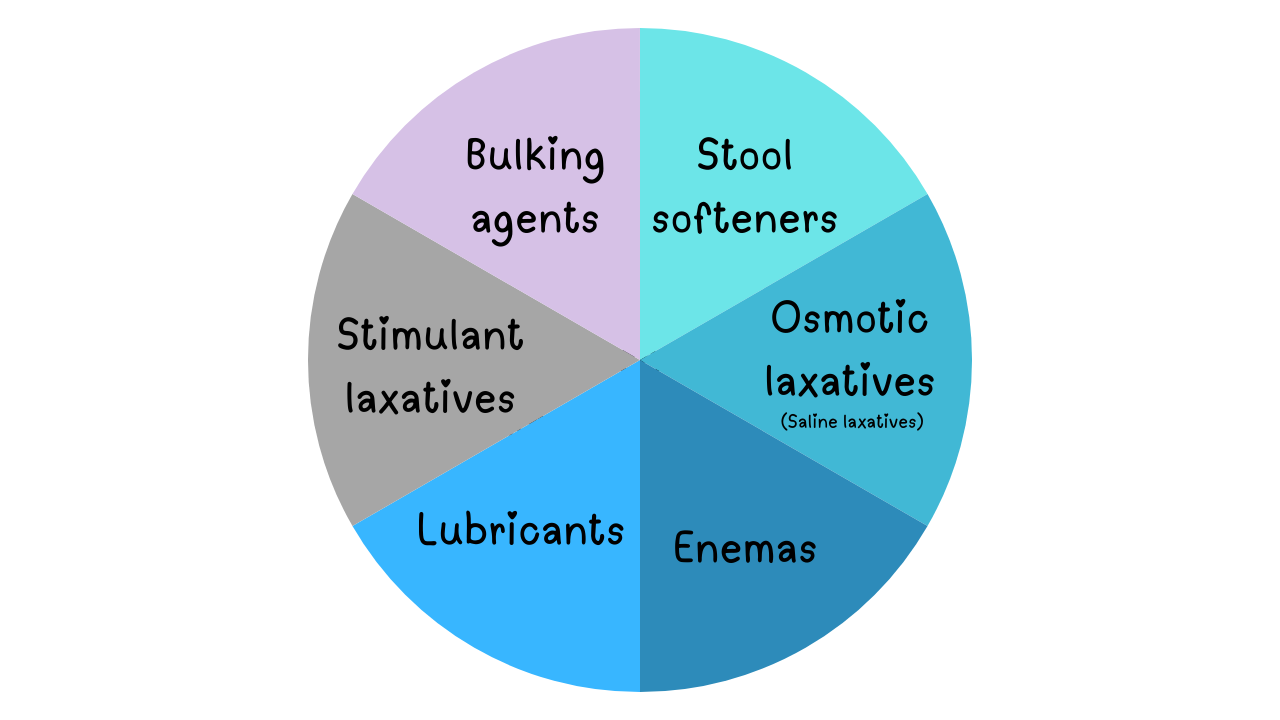
Bulking agents
- The gentlest.
- Add soluble fibers to the stool which draws water into your stool, making it bigger and softer, in turn, this will stimulate the colon to contract and push the stool out.
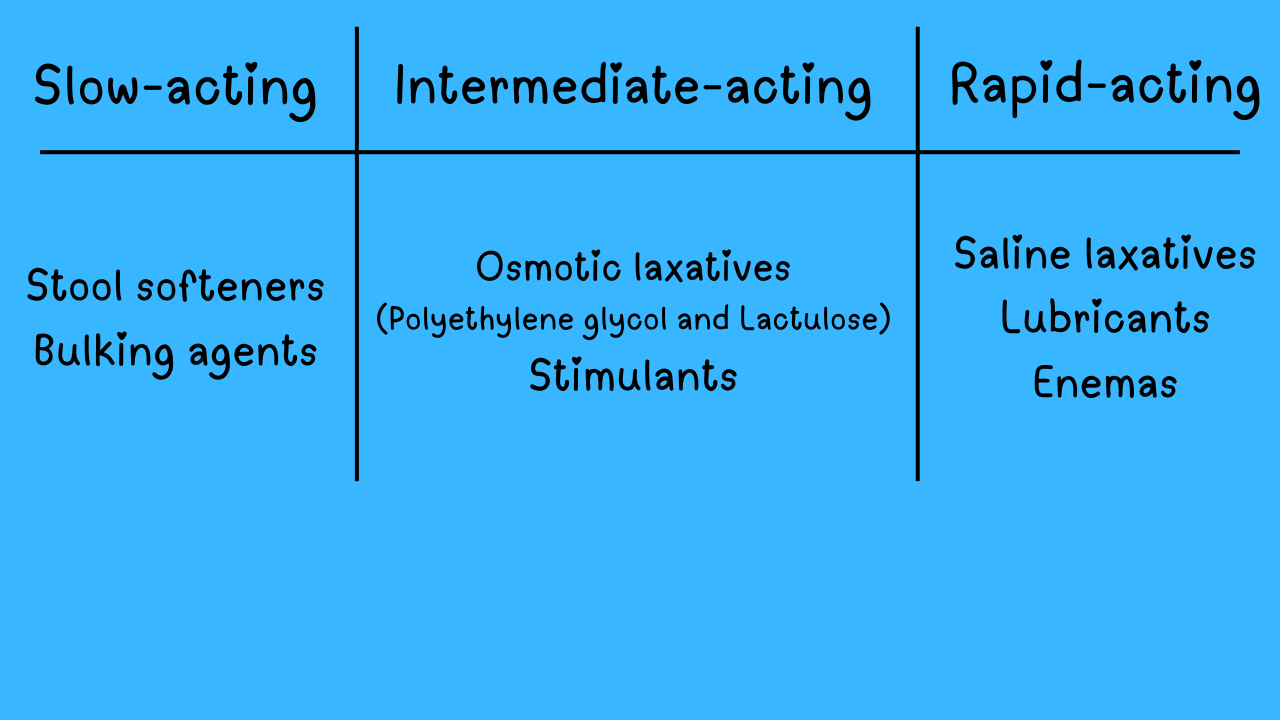
- Slow-acting, effect is seen from 12-72 hours from administration.
- Examples of bulk agents are psyllium seed (eg, Metamucil) and Methylcellulose (Citrucel®).
Stool softeners
- Increase the water and fat the stool absorbs, softening it.
- Slow-acting, effect is seen from 12-72 hours from administration.
- An example of this is Docusate sodium.
Osmotic laxatives
- Draw water into the lumen to increase intestinal peristalsis. As the water collects, it softens the stool so it’s easier to pass.
- They typically work within 1-2 days.
- Examples of this are Polyethylene glycol and Lactulose.
Saline laxatives are a more potent type of osmotic laxatives. They contain salt that holds water in our colon. They are fast-acting and typically work within hours. Examples are magnesium hydroxide (milk of magnesia) and Magnesium citrate.
Stimulant laxatives
- Activate sensory nerve endings to promote colonic motility and reduce colonic water absorption.
- Fast-acting and typically work within 12-24 hours.
- Examples include bisacodyl and senna.
Lubricant laxatives
- Coat our colon, making it slick. The coating prevents your colon from absorbing water from your stool, so it stays soft. It also makes for a slippery passage that makes pooping easier.
- Fast-acting and typically work within hours.
- An example of this type is mineral oil.
Enemas
- A last resort option
- the fastest to work.
- An example of this is sodium phosphate and saline enema
Laxatives forms
- Pills as in docusate sodium, bisacodyl, and senna.
- Powder as in Polyethylene glycol and Metamucil.
- Liquids and syrups as in lactulose, magnesium hydroxide, magnesium citrate, and mineral oil.
- Suppositorie as in bisacodyle.
- Enemas such as sodium phosphate enema, bisacodyl enema, and saline enema.
Laxatives potency
How to help a Constipated patient in inpatient settings
- Apply the first 4 steps we mentioned earlier – if not applied already
- Ambulation
- Adequate hydration
- Optimizing electrolytes
- scheduled bulking agent or a stool softener: Metamucil 30 gm/day all at once or in divided doses can be used as a bulking agent, or docusate sodium 100 mg BID as a softener.
- If the patient requests something relatively mild and not quick, I add a scheduled osmotic laxative such as lactulose 30 ml every 6-8 hours or Polyethylene glycol 17 gm daily. I also have them drink prune juice if possible.
- If the patient requests something stronger and has a BM within 24 hours, I add a scheduled stimulant laxative such as Senna 8.4 mg one tab orally BID, or bisacodyl 10 mg orally once daily.
- If the patient requests something quick and strong, saline laxatives (magnesium hydroxide or citrate) are the ones I go for, mg hydroxide or mg citrate 30 ml every 8 hours x2 days or until a BM.
- For severe cases, I go for one of these three options:
- Mg citrate 30 ml every two hours until BM or finish the whole bottle of 300 ml.
- To drink four gallons of polyethylene glycol (Golytely) which is mainly used for colon prep before colonoscopy.
- Use an enema, sodium phosphate, and saline enema.
- Once BM is achieved, I change osmotic or stimulant laxatives from scheduled to PRN/as needed only. But we keep bulking agent/ stool softener whichever we used as scheduled.
- Stool impaction needs manual disimpaction or enema, otherwise, it will be very hard to have a BM with oral laxatives.
Precautions and contraindications
- Avoid magnesium products in patients with advanced renal failure (creatinine clearance is < 30 ml/min) who are not on dialysis yet.
- Magnesium laxatives may be used in compliant dialysis patients.
- Abdominal cramps and bloating are some of the manageable common side effects of most laxatives.
- Diarrhea may develop with any laxative. Ask your patients daily about bowel movements. Discontinue all kinds of laxatives including bulking agents and stool softeners. In most cases, diarrhea will resolve within 1-2 days.






The top three antiemetics I rely on!
The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications
Chest Tubes & Pigtails: 5 Must-Know Tips for ICU Rotation
Mechanical Ventilation Made Simple: 9 Concepts Every Non-ICU Doc Should Know