The hospital is one of the worst places to sleep in for many reasons; different environments, different beds, beeping pumps, screaming patients, early morning blood work, and vital sign checks.
Some hospitals may try to minimize that by adjusting the time for vital sign checks and blood work, having nurses respond to alarms quickly; closing patient doors; enforcing visiting-hour restrictions; and posting “quiet” signs.
While covering the floor, we don’t have the luxury of getting a thorough sleep history or trying behavioral therapy! That is appropriate for outpatient chronic insomnia treatment. In the hospital, when patients ask for help to sleep, they expect to receive medication for that!
Insomnia drug classes
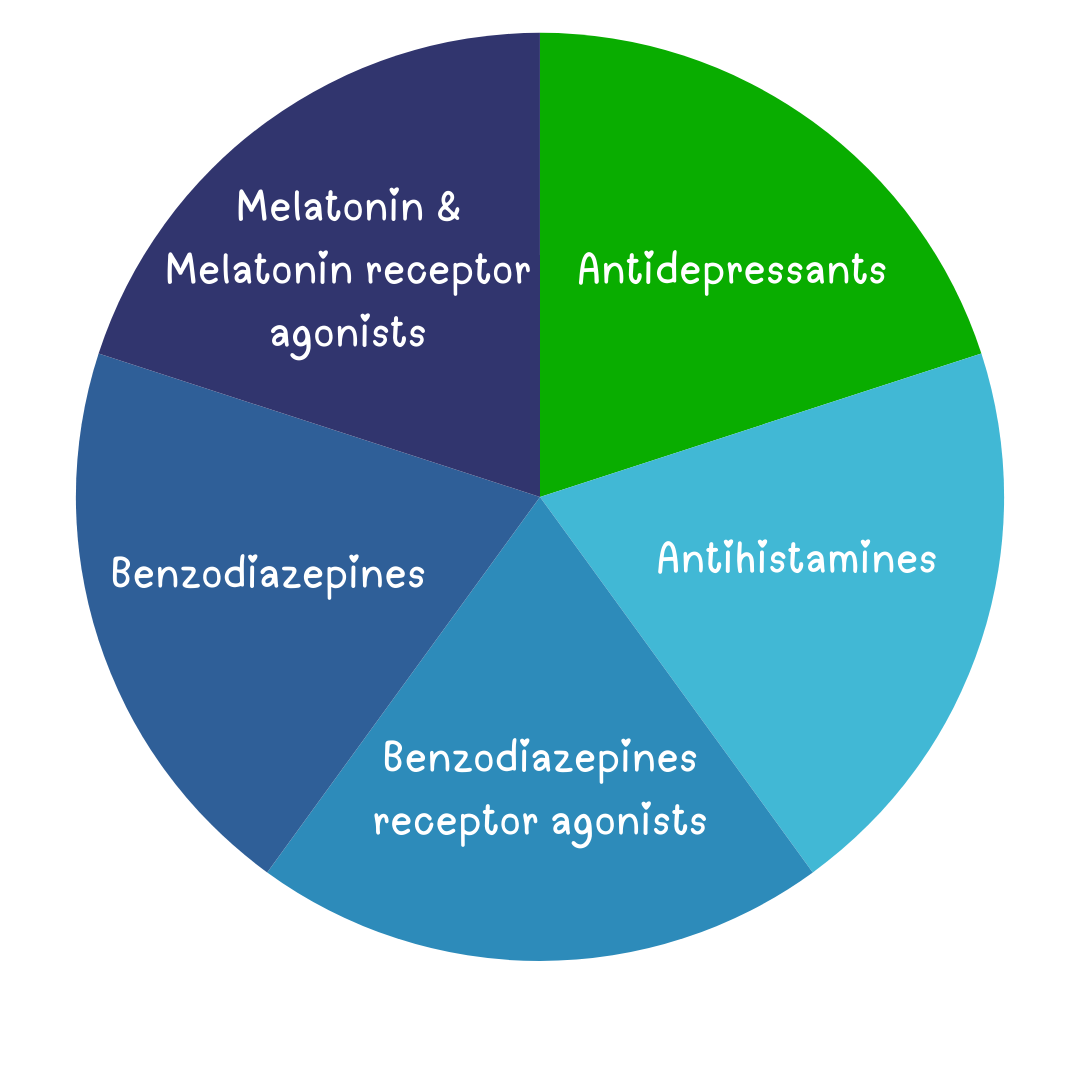
Melatonin & Melatonin receptor agonists
- Melatonin is available in almost all US hospitals
- First-line option.
- Melatonin 3, 5, and 6 mg at bedtime can be prescribed.
- Melatonin receptor agonist ramelteon is not available in most hospitals’ formularies, if it’s available, ramelteon 8 mg as needed at bedtime can be prescribed.
Antidepressants (Trazodone & Mirtazapine)
- Trazodone and Mirtazapine are the antidepressants that are widely used as insomnia drugs.
- Trazodone 50-100 mg is commonly used for insomnia, a lower dose of 25 mg should be used in elderly patients.
- QTc prolongation, orthostatic hypotension, nausea, and headache are important side effects of Trazodone. Trazodone should be avoided if there is a prolonged QTc or drugs known to prolong QTc.
- Mertazapine at lower doses of 7.5-15 mg may be used as an insomnia drug but it stimulates appetite which can be good for some and not for others.
Benzodiazepines receptor agonists (Zolpidem)
- It helps with sleep onset and sleep maintenance.
- Use 5 mg in females and the elderly, and 10 mg in younger adults.
- Zolpidem is the drug of choice in pregnancy and breastfeeding.
Antihistamines
- Diphenhydramine/ hydroxyzine/doxylamine 25 mg orally as needed at bedtime may be prescribed.
- Avoid in patients older than 60 given its anticholinergic side effects causing delirium and urinary retention.
Benzodiazepines
- Temazepam (Restoril) may have the best safety profile for use in insomnia.
- It helps with sleep onset and sleep maintenance.
- Temazepam 7.5 or 15 mg PO can be prescribed.
Which one to use
- Check if the patient takes something at home and resume it if there is no contraindication.
- If the patient asks for a specific insomnia drug, that worked for them in the past, we can order that specific agent if no contraindication.
- If the patient isn’t taking any insomnia drugs at home:
- Melatonin or melatonin receptor agonists are the first line.
- Trazodone is the second line.
- zolpidem comes third.
- Temazepam and dephenhydramine come last.
How to use
- Start with the lowest dose available particularly in elderly patients.
- Use immediate-release forms, and avoid extended-release forms in inpatient settings.
- Insomnia drugs should be ordered PRN (as-needed basis) at bedtime, not scheduled.
- Avoid giving insomnia drugs with other sedatives simultaneously or close to each other, for example, don’t give morphine and diphenhydramine at the same time or close to each other.
- Pay extra attention to obese patients, patients with OSA, and patients with advanced pulmonary diseases. These patients should be placed on continuous pulse oximetry.
- Insomnia drugs should not be ordered routinely as part of the order set. Please don’t order it unless the patient asks for help to sleep.
- Almost all insomnia drugs may cause – with variable degree – drowsiness and prolonged sedation which can lead to imbalance and increase the risk of falls. This is more prominent with Benzodiazepines, benzodiazepine receptor agonists, and antihistamines, all of which increase the risk of delirium as well.
- I highly recommend against discharging the patient on these insomnia drugs! If they ask for a prescription on discharge, advise them to follow up with their primary care physician for a more thorough insomnia assessment and treatment.
- If you decide to write them a prescription, don’t give more than three days’ supply.






Eight EKG patterns in acute MI we can’t afford to miss!
The top three antiemetics I rely on!
The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications
Chest Tubes & Pigtails: 5 Must-Know Tips for ICU Rotation