Most incoming interns may feel overwhelmed in the first few weeks and some even in the first few months which everyone will tell is normal! but you don’t have to! In this post, I will discuss types of clinical rounds, rounding sequences, rounding checklist, and writing a progress note.
Types of clinical rounds
- Official main round: this is the round with your attending physician.
- Early round: This is your own round on your patients preparing for the official round.
- Late round: This is a round to follow up on your patients later during the day.
Although, as an intern, your day officially starts with meeting the night team to get the sign-off, many interns may start well before that to finish their early round before the official round starts.
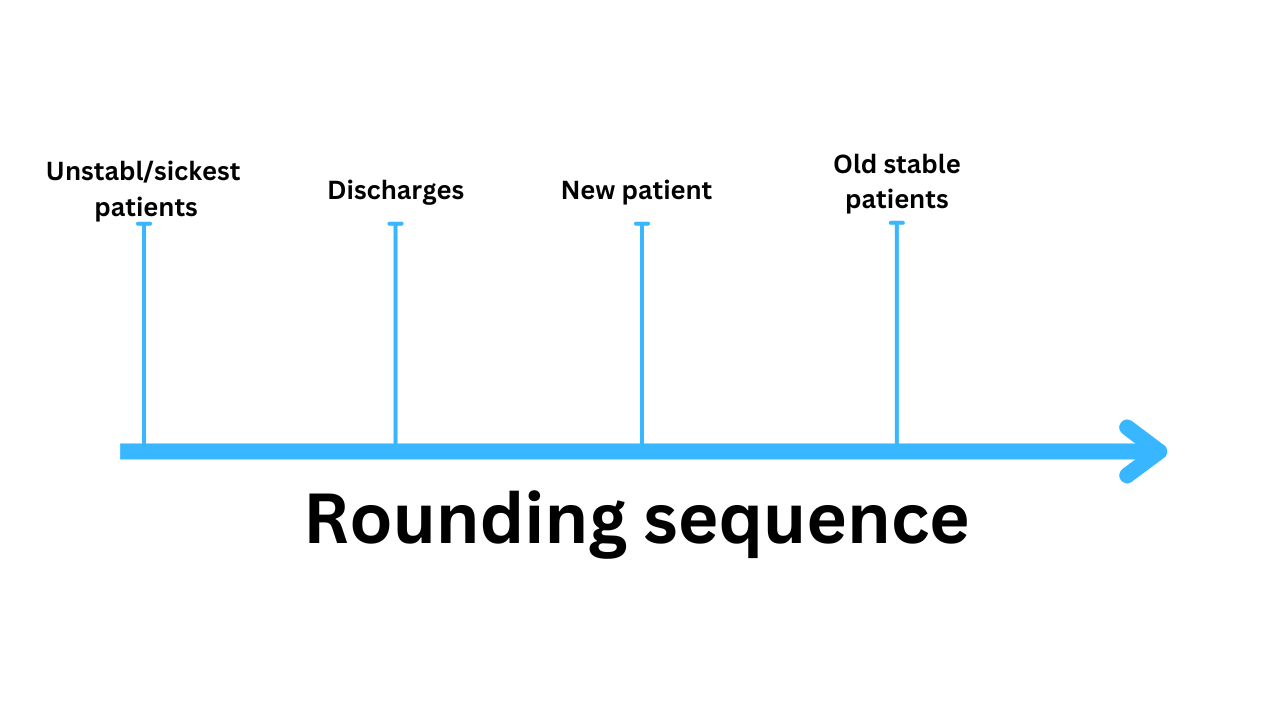
Rounding sequence:
The patients on your list fall into one of the following categories:
- The unstable/sickest patients.
- Patients who are likely to be discharged.
- New Patients.
- Old, stable patients who are unlikely to be discharged.
Unstable patients
Patients with unstable vital signs or having active concerning symptoms. An ICU patient doesn’t necessarily mean an unstable patient.
Active concerning symptoms: active chest pain, altered mental status, shortness of breath, rectal bleeding, hematemesis, severe acute back pain, severe abdominal pain,..etc. These symptoms may be associated with relatively normal vital signs initially so don’t be deceived.
Examples:
Example (1): An ICU patient on mechanical ventilation day 2, stable vital signs on low dose Norepinephrine, and his ventilator settings remained stable.
Example (2): A floor patient with active chest pain.
Example (13): A floor patient was on RA last night but is now on 8 L of O2, his O2 sat is 97%, RR 22, HR 101, BP 145/87, T 98.
Which one needs immediate attention?
The ICU patient is considered stable with stable vital signs and stable ventilator settings, being on low-dose epinephrine isn’t uncommon in ICU.
A patient with active chest pain is definitely someone who needs immediate attention.
The third patient has stable vital signs but now with significantly increased oxygen demands. Hence, he needs attention to prevent any further deterioration and correct hypoxia but only after we see the patient with active chest pain.
So I would see the patient with active chest pain first, the patient with increased O2 demands second, and the ICU patient third.
Rounding checklist
“Please have a clipboard or whatever you like to use, you need to write things down, don’t trust your memory”
Download the checklist: https://rahamneh.gumroad.com/l/roundingchecklist
The following checklist is a step-wise approach to ensuring effective rounding:
- Before heading to your early round, review your patients’ labs, cultures, imaging, and medications. Don’t forget to document I&O in patients undergoing diuresis. Skip this step if a patient is unstable! Go see them immediately.
- Place necessary orders based on the results of labs, cultures, and imaging.
- Review telemetry information if indicated.
- Before heading to the patient’s room, talk to the patient’s nurse, ask the nurse about any important overnight events, and if possible have them see the patient along with you.
“Have a chaperone with you, particularly when seeing a patient from an opposite gender”
- Review any signs on the door of the patient’s room. Signs may include isolation signs, NPO signs, fluid restriction signs, and maybe some visitor restrictions signs. You must know why each sign is there and if the indication isn’t valid anymore, please discontinue that.
- Knock the door, Greet the patient, and introduce yourself and what your role is if it’s the first time meeting the patient. We may need to do this daily with forgetful patients.
- While greeting the patient take a quick inspection of both sides of the bed, and the whole room, and watch for the following:
- If there is anyone else in the room, identify them and If they are not an immediate family member, make sure the patient is comfortable speaking in their presence.
- The general feeling of the patient: is the patient comfortable, sleepy, restless, angry, in pain, in respiratory distress,…etc.
- Is the patient on O2, what kind, and how much: is it regular NC, vapotherm, CPAP,…etc? Ask if the patient uses home O2 and compare it to the current amount. Wean the patient off O2 as soon as you can, and add IS if feasible.
- Is there a Foley catheter? Remove it if no valid indication.
- Any hung bags? IV fluid, IV antibiotics, or other drips? Discontinue them if not indicated, particularly IV fluids, I see them hung all the time and nobody bothers to stop them.
- Any meal tray? See how much is left of their meals. A good appetite is always a good sign!
- In the ICU, you must read the monitor and document all the info (rhythm, CVP, EtCO2, PAP).
- After that, grab a chair if feasible, sit down, and ask two types of questions:
- Questions related to the patient’s active problem. For example, for a patient who just had a coronary stent, we must ask if they have chest pain, shortness of breath, nausea, vomiting, or feeling dizzy or lightheaded. I will not necessarily ask about dysuria or urinary frequency.
- Questions related to the well-being of the patient: How was your night? Did you sleep well, how’s your appetite, any BM, and when? Are they getting out of bed?
- Get up and examine the patient, and like with questions, there are two types of physical examination:
- Focused physical exam related to the active problem, for example, a patient with a stroke should have a neurological exam, and a patient with cellulitis should have the cellulitic area examined while may not necessarily need a neurological exam. Or a patient who had a left heart cath through femoral access a day earlier, examining their groin and feeling the femoral artery pulse becomes paramount.
- The “Listen & feel” physical exam regardless of what the active problem is and includes the following: A quick listen to their hearts and lungs, feel the abdomen, don’t forget to palpate the urinary bladder, especially in elderly male patients to detect urinary retention, and feel the legs for signs of edema, check both legs and don’t skip the feet.
- Explain your plan for the day to the patient, this is the most powerful tool to make patients feel they are in control of their health which improves satisfaction scores! Here is where you update the patient about test results and the plan of the day.
The plan of the day should include:
- Any planned tests or procedures.
- Any planned treatment for the day including:
- Starting new, continuing, or discontinuing medications including IV fluids
- Weaning of O2 or other breathing machines,.
- Discontinuing or adding equipment (foley catheter, NGT, rectal tubes, or the use of IS.
- Chnage in diet or NPO status.
- Ambulation, physical therapy
- The estimated day of discharge and where to: always tell them it’s an estimation and never give a specific date!
Always tell them you will discuss the plan with the attending physician so things may change. Inform them you will be back with the team later on.
Example:
You are rounding on a patient with CAP on IV antibiotics who is on 4 L of O2, the patient doesn’t use home O2, and is feeling better.
My plan would be something like this: I am glad you are feeling better, today we will try to completely wean you off oxygen, I want you to start using IS, will continue the same IV antibiotic for another day, I want to get you out of bed and having PT help you walking in the hallway with PT, I am anticipating you will be going home in the next 24-48 hours.
- Before you leave, ask if they have any questions
After you leave the room, write the following:
- Relevant pieces of the history and physical exam for your patient’s presentation and writing your notes later.
- Write any orders you need to place, later on, urgent orders should be placed immediately.
Download the checklist: https://rahamneh.gumroad.com/l/roundingchecklist
Next is the official round with your attending! During these rounds, ensure that you or a team member takes notes on the attending physician’s recommendations to address them afterward. Many orders and recommendations can be implemented during the rounds if the attending physician allows it. Some physicians prefer that the entire team remains fully focused on the round.
Progress note
Before working on your notes, Ensure discharges/orders/follow-ups are done.
“Don’t be obsessed with finishing your notes! Finish your tasks first”
With electronic EMR, most copy the notes from the day before which is a good way to save time but you must update it for the day.
If you are writing the patient’s first progress note, it will take you a bit longer! EMR will provide you with progress notes templates or you can create your custom notes. Regardless a progress note must have the following elements:
- Update on the active problems-related symptoms.
- Physical exam.
- Relevant labs and diagnostic results.
- Assessment and plan ( We must include all the problems we are actively treating including chronic conditions).
Late round
The late-round is an optional informal quick round to follow up on your remaining patients, update them on any test results, and check with case managers or discharge planners for next-day discharges which I will discuss in the discharge video.






Transfusion Medicine Made Simple: Essential Guide for Clinicians
Eight EKG patterns in acute MI we can’t afford to miss!
The top three antiemetics I rely on!
The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications