Brief physiology
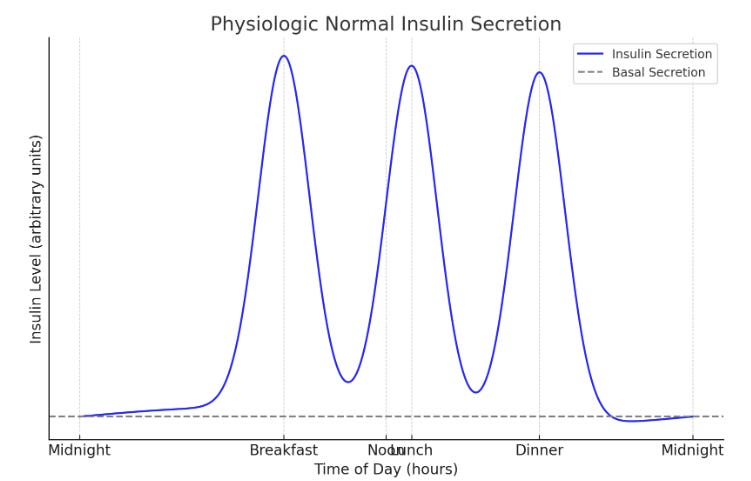
- Physiologic normal insulin secretion is characterized by continuous basal secretion with peaks or blouses that occur soon after meals.
- With insulin therapy, we try to mimic that by giving basal/bolus insulin therapy:
- Basal insulin to control the blood sugar overnight, while fasting, and between meals.
- Bolus insulin to control the post-prandial rise in blood glucose.
Insulin classification:
Insulin is classified in two ways:
- Based on the way it’s synthesized:
- Human regular insulin.
- Insulin analogs.
- Based on the duration of action:
- Short or rapid-acting (Bolus).
- Intermediate-acting (Basal).
- Long-acting (Basal).
Human vs analog insulin
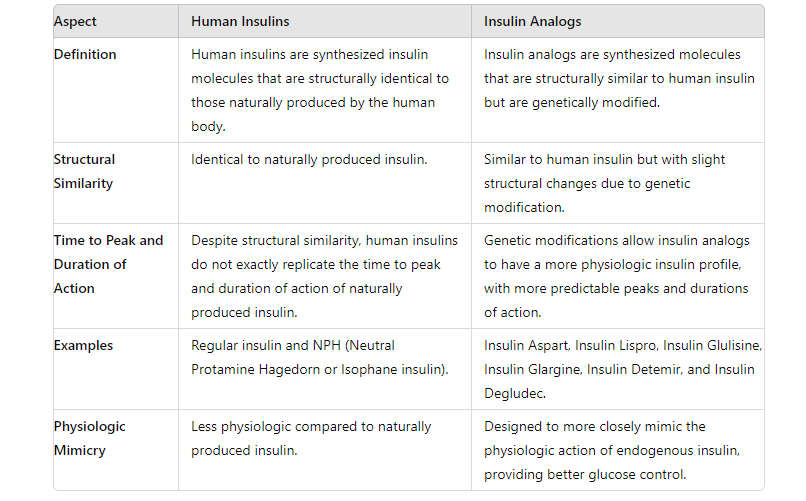
Insulin analogs mimic endogenous insulin physiology more than human insulins.
Pick insulin analogs over human insulins unless IV insulin is required as in treating hyperkalemia or when insulin drip is required where regular human insulin is preferred.
Human regular Insulin and Glulisine insulin come in IV form as well. IV Glulisine insulin is expensive and not widely available.
Basal vs bolus insulin
- Bolus insulin is used to control the post-prandial rise in blood glucose and should have the following characteristics:
- A rapid onset of action.
- A short duration of action.
- Should be given before meals, whether as scheduled before meals (AC) or as needed correction sliding scale.
- All short/rapid-acting insulins are considered bolus insulins including human regular insulin, and insulin analogs ( Insulin lispro, Insulin aspart, and insulin glulisine).
- Basal insulin is used to control blood sugar overnight and while fasting and should have the following characteristics:
- A slow absorption and onset of action.
- A long duration of action.
- Administered once or twice daily.
- Intermediate and long-acting insulins are considered basal insulin including NPH, Detemir, Glargine, and Degludec.
Bolus insulin
- Human regular insulin:
- Has a delayed onset of action resulting in a need to inject it at least 30 minutes before the meal to best cover post-meal glycemic hyperglycemia which is inconvenient for many diabetic patients.
- Has a duration of action that exceeds the duration of the postprandial rise in glucose observed after most meals, particularly meals that are not high in carbohydrates and fat, therefore hypoglycemia may develop several hours after eating, this can be prevented by eating a snack.
- Administered SQ or IV.
- Insulin analogs:
- Enter the bloodstream within minutes, so it is important to inject them right before or within 5 to 10 minutes of eating.
- They have a peak action period of 1-2 hours and fade completely after about four hours. less risk of hypoglycemia compared to human regular insulin.
- Preferred for mealtime bolus insulin and correction sliding scales (Please use them over human regular insulin).
- All administered SQ. Glulisine comes in IV form as well.
IV bolus insulin is used in two situations:
- When insulin drip is required as in DKA, NKHH, or critical hyperglycemia.
- In the treatment of hyperkalemia.
Scheduled pre-meal bolus insulins should only be given to patients with adequate oral intake. Give clear instructions to avoid administering the premeal bolus insulin unless the meal tray is present in the patient’s room and the patient must consume it.
Basal insulin
- Intermediate-acting (NPH insulin).
- Long-acting (Detemir, Glargine, and Degludec).
- Continuous subcutaneous insulin infusion (Insulin pump).
Intermediate-acting insulin:
- Has a duration of action is up to 12 hours.
- Administered twice daily.
- NPH human insulin (Neutral protamine Hagedorn or isophane insulin) is the only one in this category.
- NPH is a suspension of different-sized crystals and has a very unpredictable absorption rate and action leading to more frequent low and high blood sugars.
The use of long-acting insulin analogs is preferred over intermediate-acting given its more predictable course.
- NPH is the only basal insulin that can be mixed with rapid-acting insulin. The available premixed insulin solutions in the United States are:
- NPH+Lispro mixed at 50:50 (50% NPH and 50% insulin Lispro) or 75:25 (75% NPH and 25% insulin Lispro ) ratio.
- NPH+Aspart mixed at 70:30 mixtures (70% NPH, 30% insulin aspart).
- NPH+Regular human insulin mixed at 70:30 (70% NPH, 30% Regular).
- Despite its convenience, it’s preferred to use long and rapid-acting insulins separately to get more predictable and more reliable results.
- Premixed insulin can be a good option for those who need a straightforward treatment plan.
Long-acting insulins
- Long-acting insulin analogs are absorbed slowly, have a minimal peak effect, and have a stable plateau effect that lasts most of the day.
- Administered once or twice daily.
Long-acting insulins: Detemir, Glargine, and Degludec.
- Insulin detemir (brand name Levemir):
- Has a duration of action of 12-24 hours.
- Twice daily administration is better for optimal glycemic control.
- Insulin Glargine:
- Has a duration of action of 24 hours.
- There are two types of glargine available in the market:
- Glargine U- 100 (brand name of Lantus, Basaglar, or semglee).
- Glargine U- 300 (brand name Toujeo).
- The more concentrated U-300 form has a longer duration of action and is given once daily.
- The U-100 has a less duration of action and can be given once or twice daily.
- The conversion ratio between glargine U-100 and U-300 is 1:1.14, if a patient is taking 100 units of glargine U-100, he will need 114 units of glargine U-300.
- The conversion rate between Lantus and Basaglar or Semglee is 1:1.
- Insulin degludec (brand name Tresiba):
- Has the longest duration of action among FDA-approved long-acting insulin analogs with a duration of action > 40 hours (Ultra-long-acting).
- Given once daily.
- Available in U-100 and U-200. The conversion ratio is 1:1.
- U-200 is used in those with high insulin requirements.
- The continuous subcutaneous insulin infusion ( Insulin pumps):
- Almost exclusively used in type 1 diabetics.
- Filled with rapid-acting insulin analogs.
- The pump is programmed to provide the patient with an hourly infusion rate (basal rate), and mealtime/ high blood sugar correction insulin replacement (Bolus).
Logistics
- Human insulins are cheaper compared to insulin analogs and can be a good option for those without insurance or those with a large copay.
- Injectable insulin is available in prefilled disposable insulin pens, reusable insulin pens with disposable insulin cartridges, or in vials.
- Insulin pens come preloaded with insulin and are more convenient to use than insulin vials with syringes because they combine the medication and syringe in one handy unit, of course, pens are more expensive!
- Insulin syringes are available in 0.3, 0.5, and 1 mL sizes. The 0.3 mL syringe is useful if the insulin dose doesn’t exceed 30 units; the 1 mL syringe is used for insulin doses up to 100 units.
- When using insulin pens or vials with syringes, the shortest available needle is recommended (eg, 4 or 5 mm for pen needles) to avoid intramuscular injection and to minimize discomfort and tissue damage.
- Insulin can be injected into the abdominal wall, leg, arm, or buttock.
- Human insulins are absorbed fastest from the abdominal wall, slowest from the leg and buttock, and at an intermediate rate from the arm. These differences can be useful clinically:
- Pre-meal regular insulin should be rapidly absorbed, and injection into the abdominal wall may therefore be preferable.
- Rapid-acting insulin absorption is increased when the insulin is injected into an exercising limb due to increased blood flow.
- Pre-evening meal dosing of intermediate-acting insulin should be slowly absorbed to ensure a duration of action that lasts through the night, and injection in the leg or buttock may be preferable.
- The absorption of the long-acting basal insulin analogs, glargine, and degludec, do not appear to be significantly influenced by the injection site.






Transfusion Medicine Made Simple: Essential Guide for Clinicians
Eight EKG patterns in acute MI we can’t afford to miss!
The top three antiemetics I rely on!
The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications