Three questions we must ask every time a nurse calls about a patient with high blood pressure:
- What are the rest of the vital signs?
- Does the patient have any signs and symptoms?
- Is the patient pregnant and what trimester? Of course, only ask this if the patient is a woman of childbearing age.
If the patient’s vital signs are unstable, they are showing concerning signs or symptoms, or they are pregnant, stop what you are doing and see the patient immediately. This situation constitutes a hypertensive emergency, which we will discuss in our next post.
If the rest of the vital signs are normal, the patient has no symptoms, and they are not pregnant, there is no emergency. This is the most common scenario you will encounter while covering the floor.
“Check the patient’s BP trend over the previous 48 hours or whatever BP values are available to compare to see if this elevated BP value is a single isolated out of the trend value or not”
Noninvasive BP measurement
- There are two non-invasive ways to measure BP:
- The auscultatory method (the manual one).
- The oscillometric method using the machine.
- Both are fairly accurate, the oscillometric method isn’t operator-dependent but has not been validated when checking BP on the leg.
- Suspect a BP measurement error if the elevated BP value was a single isolated, and of the trend value, in such a case, kindly recheck the BP, if the value is still high, is it still possibly a measurement error?
- There are two main reasons for noninvasive BP measurement errors:
- Inappropriate cuff size.
- Inappropriate cuff position.
- The appropriate cuff size should be 80% long, and at least 40% wide of the circumference of the upper arm.
- Suspect a small cuff size issue if the DBP is markedly elevated with a narrow pulse pressure.
- The arm is the standard place to measure BP, we should place the cuff just above the cubital fossa, the cuff should also be placed on the bare arm or over a thin sleeve, don’t roll up the sleeve or place the cuff over a thick sleeve, please!
- When the arm can’t be used to measure BP due to the presence of an arm fistula, graft, indwelling catheter, or surgery, the wrist or the leg can be used.
- If we use the wrist make sure to keep the wrist at the level of the heart, otherwise, the BP may be falsely elevated if the rest is below the heart.
- If we use the leg, the systolic pressure in the lower extremity is usually higher than that in the brachial artery, except in PAD and aortic coarctation cases where the pressure at the leg is lower than in the arm, However, overall it is difficult to reliably translate leg pressure into arm pressures so use only if there is no other option or if you are checking the ankle-brachial index.
Treatment
- For the sake of the treatment, we will categorize patients into three groups based on their BP readings:
- Patients with SBP < 160 & DBP < 100
- Patients with SBP < 180 & DBP < 120
- SBP > 180 and/or DBP >120
- For all patients with high BP (STEP 1):
- Place them on a low-sodium diet.
- Ensure the patient’s home BP medications have been resumed with the correct doses unless the patient is strictly NPO or there is a contraindication to restart home BP medications.
SBP is <160 and DBP < 100
- Perform step (1).
- No additional steps are needed, don’t give any PRN BP medications! Refer patients for Outpatient f/u for further evaluation.
SBP 160-180 & DBP 100-120
- Perform step (1).
- If the patient was already on a low-sodium diet and the correct doses of home medications, simply adjust home medications or add a new long-acting agent to the patient’s regimen.
- No need to give PRN IV or oral BP medications.
- The goal is to lower SBP < 160 and DBP < 100.
SBP > 180 and/or DBP >120
- The BP is significantly high and we need to lower it over the next few hours.
- Give an oral short-acting agent to bring the BP down over the next 4-6 hours.
- IV BP medications are reserved for:
- Patients who are strictly NPO.
- Patients who are very anxious about their high BP and want to lower their pressure much faster.
- The goal is to lower SBP < 180 and DBP < 120.
Follow up
- Recheck the BP within 4-6 hours after a short-acting oral agent is administered.
- Recheck the BP within an hour after an IV agent is administered.
- If the BP remains above the target we give another dose of the same medication at the same or higher dose or we pick another class if there was no response at all to the first one.
- Adjusting the patient’s BP regimen or adding a long-acting BP medication can be done at the same time as well
Short-acting PRN agents:
- The most commonly used oral agents in practice are clonidine & captopril, please don’t sublingual nifedipine at all!
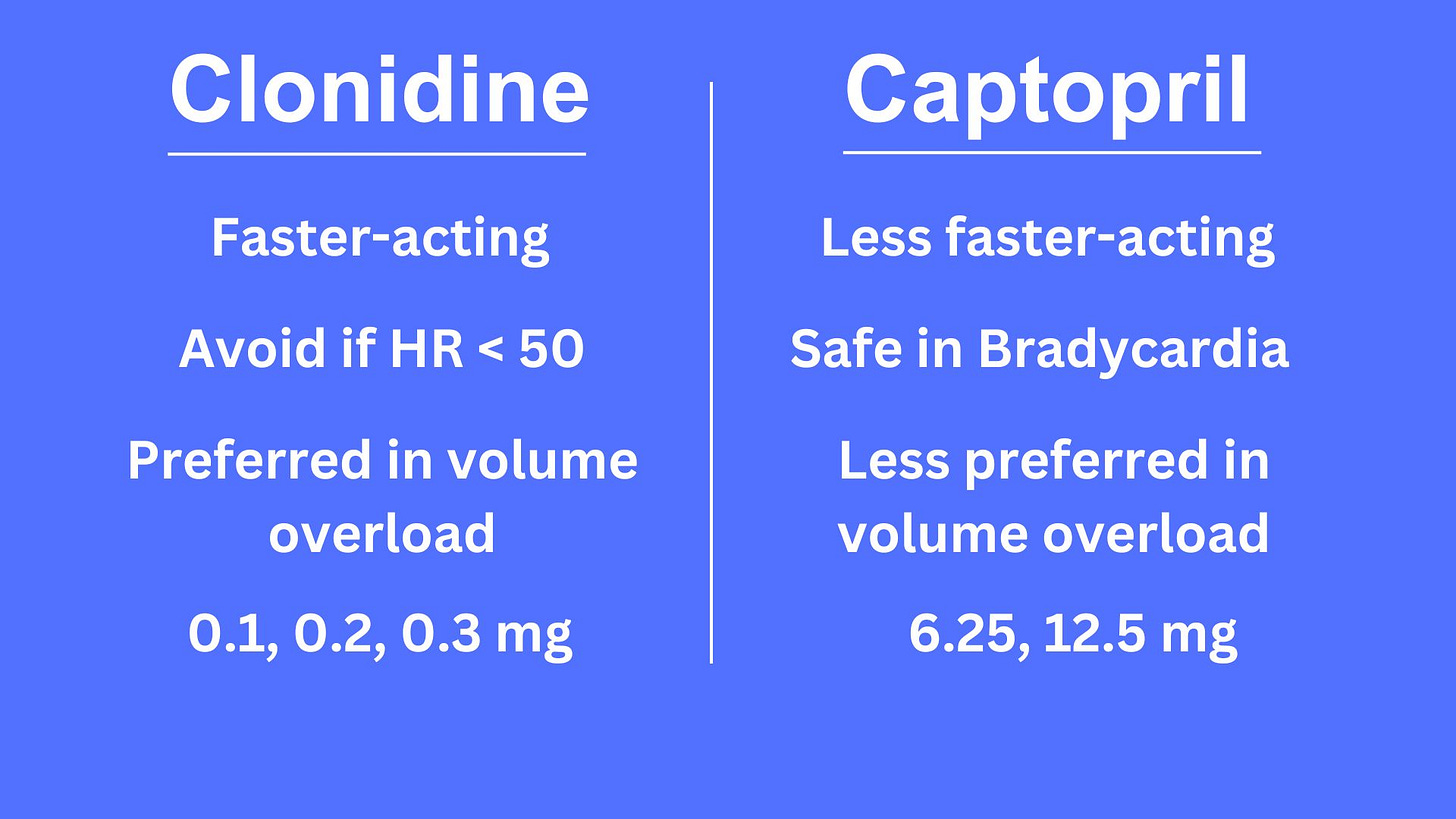
- Clonidine patch is a long-acting medication that does not help lower BP quickly so don’t use it, please!
- The most commonly used IV medications used in practice are labetalol/hydralazine or enalaprilat.
- 20 mg of IV labetalol, 10 mg of IV hydralazine, or 1.25 mg of IV enalaprilat can be used.
- Labetalol should be avoided if HR < 50, hydralazine can cause reflex tachycardia in the low 100s.
- Enalaprilat is to be avoided if allergy to ace inhibitors, hyperkalemia, or AKI.
Long-acting PRN agents:
A Dihydropyridine-calcium channel blocker, ACE or ARBs, or a thiazide can be started.






The top three antiemetics I rely on!
The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications
Chest Tubes & Pigtails: 5 Must-Know Tips for ICU Rotation
Mechanical Ventilation Made Simple: 9 Concepts Every Non-ICU Doc Should Know