Definition
- I found the following definitions of hypotension in the literature:
- Absolute hypotension (SBP < 90 or MAP < 65).
- Relative hypotension ( a drop > 40 mmHg in SBP).
- Orthostatic ( > 20mmHg fall in SBP or > 10mmHg in DBP).
In the real-world setting, hypotension is defined by the presence of low BP (Regardelss of the absolute value) and hypoperfusion symptoms and signs, the presence of hypoperfusion signs and symptoms is essential to say the patient is truly hypotensive.
HYPOTENSION = LOW BP + HYPOPERFUSION SIGNS & SYMPTOMS.
Low BP without hypoperfusion signs and symptoms doesn’t warrant any further w/u or treatment as this is like the patient’s baseline BP.
- Check previous BP trends to see if this is the patient’s baseline BP or maybe it was just a one-off trend value which likely represents a measurement error measuring their BP.
Signs and symptoms of hypoperfusion
- All of the following may represent signs/symptoms of hypoperfusion:
- Change in mental status: the patient may develop confusion, agitation, lethargy, or obtundation.
- Chest pain.
- shortness of breath.
- Dizziness and lightheadedness.
- Low urine output, this is a difficult one to assess if urine output was not being monitored during the admission already.
- Cold, clammy, and cyanotic skin.
- Abnormal other vital signs: tachycardia, bradycardia, tachypnea, hypothermic, or hypoxia.
Every time a nurse calls us about a hypotensive patient, we should immediately ask about the rest of the vital signs and any other hypoperfusion signs & symptoms.
The presence of any sign or symptoms of hypoperfusion is a medical emergency until proven otherwise, leave everything and go see your patient right away!
Patients with mild dizziness and lightheadedness
There is a subset of patients who may only develop mild dizziness and lightheadedness, and in orthostatic patients, these symptoms may develop only upon standing, the rest of their vital signs are stable other than mild tachycardia, these patients still need to be seen and evaluated quickly. In such patients do the following please:
- Discontinue all the culprit medications.
- Keep them in bed and start fall precautions.
- Check for any ongoing volume loss like vomiting, diarrhea, bleeding,..etc.
- Initiate a fluid bolus with an isotonic solution (NS, LR, Plasmalyte).
The fluid bolus by definition should be given fast. wide open or over 30-60 minutes, especially in the elderly and in those with a history of HF.
- Monitor their BP and follow up on symptom resolution, if no improvement repeat the fluid bolus, and check for symptom resolution and the improvement in their BP.
The only true contraindication to give IVF is active pulmonary edema.
- Stop IV fluid once the symptom resolves and the BP stabilizes unless there is an ongoing volume loss like constant diarrhea, and remember to take the patient off bed rest status and start moving them with assistance.
Hemodynamically unstable patients
- Low BP with serious hypoperfusion signs and symptoms, they are in shock or going into shock, and each second counts! and can go into cardiac arrest at any moment!
- Inform the nurse over the phone that you are coming right away, meanwhile, ask the nurse to put the patient on a 100% non-breather oxygen mask, put the patient on a monitor right away if not on a monitor yet, get the crash cart into the room, and place the pads on the patient’s chest.
Call the rapid response team if your facility has this protocol! Activating a rapid response team. Rapid response can be switched to code blue if needed!
STABILIZE, RECOGNIZE, AND TREAT.:
- Stabilize the patient.
- Recognize the source of the problem.
- Treat the source of the problem.
- Don’t shy away from calling for help if you are not comfortable managing the patient yet!
- The moment I enter the patient’s room, I immediately ensure the following:
- The patient is on the monitor and the pads are on the patient’s chest.
- The patient is on a 100% non-rebreather mask if hypoxic.
- Firmly and loudly ask if there’s adequate IV access or not.
- Ask about the patient code status, is the patient full code or DNR or DNI?
- Take a glance at the monitor to check the most recent vital signs and the patient’s rhythm.
- Be firm, and loud, but respectful so everyone in the room knows you are in charge!
- The goal is to stabilize the patient to transfer him/her to the ICU.
- Remember the ABC (airway, breathing, circulation).
- Keep an eye on the monitor: check the rhythm and the BP. The BP should be checked every 3-5 minutes (remember here we are talking about a patient on the floor, not in ICU)
Stabilizing blood pressure
- Ensure adequate IV access (Two peripherals), and prepare for central line insertion.
- Give 2-3 liters of LR or 0.9 NS or plasmalyte as fast as possible, you can run two liters at the same time if the patient has two IV accesses, More IVF may be required when there is ongoing volume loss such as diarrhea, vomiting, bleeding,…etc. Recycle the blood pressure every 3-5 minutes to monitor response to IV fluid.
- Isotonic bicarb drip may be used if metabolic acidosis present ( HCO3 < 22).
The only contraindication to IVF resuscitation is active pulmonary edema! Patients will be short of breath, hypoxic, and have crackles in their chest, with or without peripheral edema.
- Start vasopressors if IV fluid is contraindicated.
- Vasopressors are reserved for the following:
- For hypotensive patients who are in active pulmonary edema where IVF is contraindicated.
- For those with extreme hypotension with SBP < 60, here I give IVF and start vasopressor simultaneously.
- For Patients with anaphylactic shock where epinephrine and IV fluid should be administered simultaneously.
- Norepinephrine is our first choice except for anaphylactic shock where epinephrine is the first choice.
It doesn’t matter if the patient has central venous access at this stage, we are trying to save the patient’s life!
- Once the patient is stable enough to be transferred to ICU, move them and don’t delay the transfer, ICU is a much better environment for such patients!
- Please remain with your patient during the transfer process, of course, along with the patient’s nurse, an ICU nurse, and a respiratory therapist, the patient should, of course, remain on the monitor, pads on, I also ask the nurse to have amps of epinephrine, calcium, and bicarb ready just in case we need to push during the transfer process
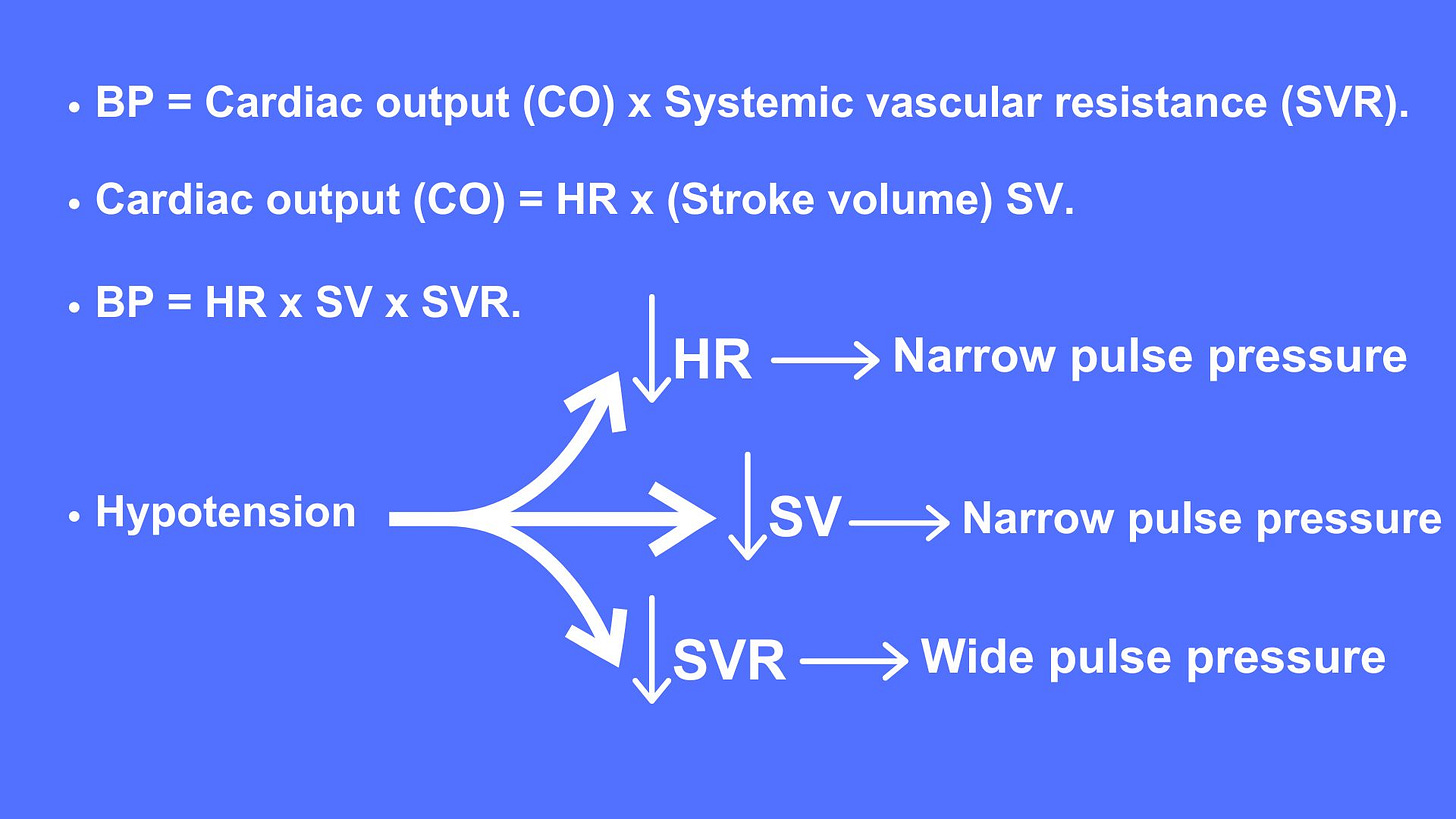
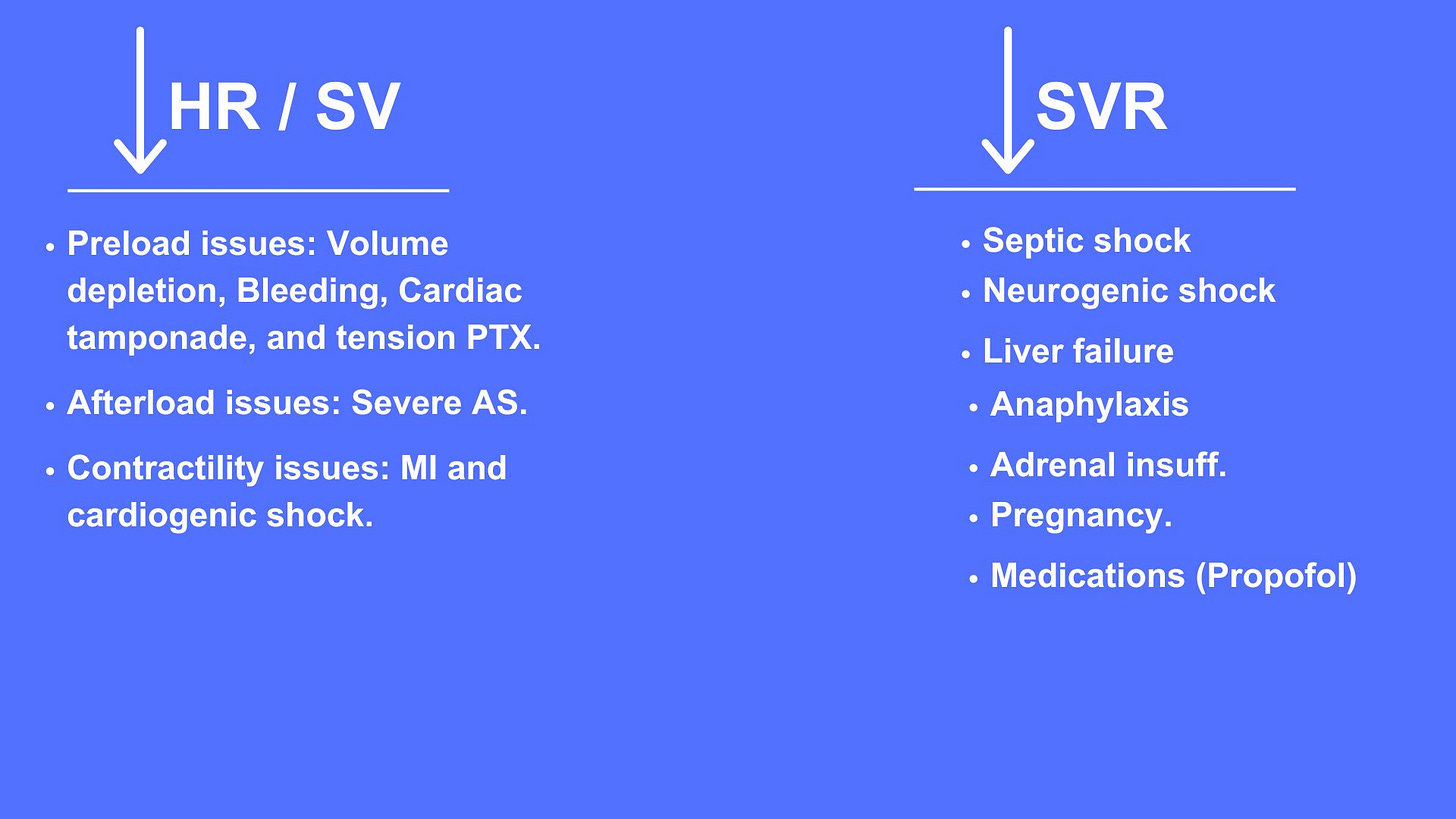
RECOGNIZE THE ETIOLOGY OF HYPOTENSION
- Two very important elements I rely on here:
- History and focused physical exam.
- And the pulse pressure (The gap between the SBP & DBP).
- Order a stat blood sugar the moment I get into the room, obtain a stat EKG, a stat CXR, an ABG, a CBC with diff, a CMP, Cardiac enzymes, lactic acids, type, and screen if bleeding suspected, further w/u with more tests may be needed like a stat echocardiogram, chest CTA if PE suspected or CT abdomen if acute abdomen suspected,..etc. remember patient needs to be stable enough to undergo a CT or MRI.
History clues
- Sudden onset shortness of breath and hypoxia, think of pulmonary edema, aspiration pneumonia, PE, or pneumothorax.
- Hematemesis, melena, rectal bleed, think GI bleed.
- Chest pain, shortness of breath, think of ACS and cardiogenic shock.
- Hypotension post CABG, think of tamponade, obtain stat echo, and inform the surgeon immediately.
- Hypotension post MI/revascularization, think of mechanical post-MI complications, obtain a stat echo, and inform the cardiologist immediately.
- Abdominal distention and diarrhea, think of Cdiff and toxic megacolon.
- Abdominal pain/hypotension, think of acute pancreatitis, acute abdomen, or intraperitoneal bleeding.
- Fever and hypotension, think sepsis and septic shock, also think of sepsis if chronic indwelling foley or foley that is in place for a few days.
- Think of transfusion reaction if the patient is receiving a blood product transfusion
- Think of anaphylaxis if hives, itching, flushing, swollen lips, tongue, or uvula.
- Remember altered mental status here is nonspecific and can happen in all.
The value of Pulse pressure
Treat the underlying problem
Initiate source treatment based on your final clinical judgment based on the process we just explained on how to narrow your differential diagnosis.






Transfusion Medicine Made Simple: Essential Guide for Clinicians
Eight EKG patterns in acute MI we can’t afford to miss!
The top three antiemetics I rely on!
The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications