Delirium prevention strategies
- Delirium is a scary experience for patients and their families! Warning them about this possibility can relieve or minimize such an experience.
- Have family on board with delirium prevention strategy:
- Ask the family to spend as much time as they can with the patient and even ask them if someone can spend the night with them.
- Ask them to provide daily orientation and redirection including reminding the patient about where they are, why they are in the hospital, what the day, time, and date,…etc.
- Ask the patient to wear his or her eyeglasses and hearing aids all the time except when they typically take them off at home.
- Ask them to keep their window shades open during the day.
- Ask them -whenever appropriate- to eat well and stay hydrated!
- Initiate delirium prevention strategy in high-risk patients:
- Remind the patient and their families to do their part in the delirium prevention strategy.
- Remind the nurses to provide daily orientation and redirection and to provide it ourselves as well when we round on these patients.
- Please write the day and date on the wall and make sure it’s large enough for the patient to see. A wall clock is highly recommended.
- Consult physical therapy early and get the patient out of bed daily, have them sit next to the window, and encourage ambulation.
- Minimize sleep interruption by:
- Setting vital signs check frequency to Q8H if possible.
- Have labs drawn at 0600 AM or later.
- Avoid or minimize Anticholinergics use (like antihistamines).
- Avoid or minimize the use of Benzodiazepines.
- Address pain control promptly preferably with nonopioid analgesia, Please minimize the use of narcotics if possible.
- Avoid constipation or urine retention, daily check for bladder distention and ask about BM
- Avoid or minimize the use of medical equipment like O2 and Foley’s catheter, please remove them ASAP if the patient becomes delirious, of course, if possible.
Delirium management
- Get a full set of vital signs and check blood sugar level when notified about a possibly delirious patient, to detect any possible life-threatening conditions that can trigger delirium. It’s also prudent to check the most recent labs to check for any major electrolyte disturbances which can also trigger delirium.
- Mildly agitated and restless patients shouldn’t be given antipsychotics, just provide reassurance and redirection! Start fall precautions, and d/c Foley’s catheter if possible.
Reassurance and redirection can be something like telling them “You are going to be okay, you are in the hospital, we are treating you for so and so, it’s so and so time and date”
- Antipsychotics are reserved for severely agitated patients who failed to respond to adequate reorientation and redirection with no other clear reversible causes.
- Antipsychotics are better given as a one-time dose rather than PRN for the following reasons:
- With PRN, patients may get antipsychotics even if they are mildly agitated or restless as this will leave it to the patient’s nurse’s clinical judgment.
- Antipsychotics should be used for the shortest time possible as they are associated with increased mortality in patients with dementia.
- Antipsychotics are considered chemical restraints that may delay patient discharge to rehab or nursing homes in the USA if it’s mentioned on the patient list of medication even if it’s PRN.
- Consider starting scheduled daily oral antipsychotics to be given right before sunset if, despite everything, the patient continues to have sundowning and agitation particularly if the patient has received antipsychotics twice or more. Please remember to discontinue that as soon as delirium has improved or resolved typically within 24-48 hours
Antipsychotics
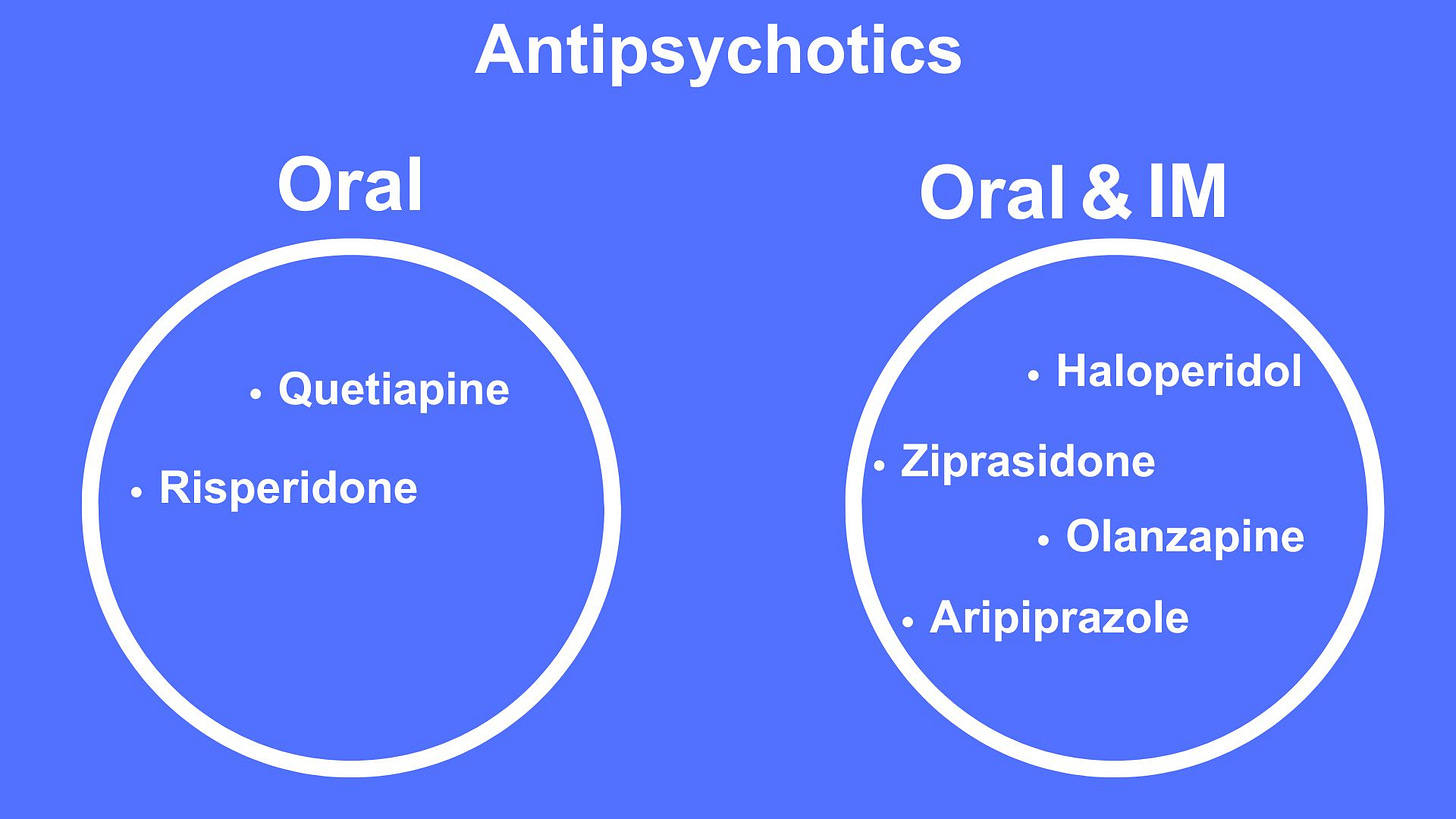
Avoid using the IV form because it’s associated with clinically significant QT prolongation.
All of them can prolong the QT interval but Aripiprazole is the one with the least effect on the QT interval.
Acute agitation:
- For IM use:
- Haloperidol 0.5-1 mg IM, the maximum daily IM haloperidol dose is 5 mg/day in non-ICU settings. In ICU higher doses of 2.5-5-10 can be given up to 30 mg/day. The dose can be repeated every 30 minutes until the patient is calm or we hit the maximum.
- Ziprasidone or Geodon can be used in 5-10-20 mg IM, repeat every 2 hours until the patient is calm or we reach the daily maximum IM dose of 40 mg.
- For oral agents:
- Quetiapine 50 mg QD is my preferred oral agent.
- Olanzapine 5 mg QD.
- Ziprasidone 20-40 mg BID.
- Aripiprazole5-10 mg QD.
- Risperidone o.25-0.5 mg and aripiprazole are good alternatives.
- In ICU settings precedex (Dexmedetomidine) drip is increasingly used for hyperactive delirium.
- If antipsychotics are contraindicated or the maximum daily amount is reached, Benzodiazepines can alternatively be used but for the shortest time possible as they are associated with worsening confusion once their effect wears out, lorazepam of 1-2 mg IV can be used. Precedex can be used in ICU settings as we just mentioned.
Please don’t:
- Use sedative antihistamines.
- Continue antipsychotic medications upon discharge! Stop them.
- Use Cholinesterase inhibitors like rivastigmine, they don’t work.
Physical restraints should be a last resort as they likely will worsen delirium as the patient becomes very frustrated with them, Try to resist placing restraints, and if you do, please discontinue them ASAP, A safer alternative is to have a 1:1 sitter, having a family member in the room can be extremely helpful.






Transfusion Medicine Made Simple: Essential Guide for Clinicians
Eight EKG patterns in acute MI we can’t afford to miss!
The top three antiemetics I rely on!
The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications