Definition
Bradycardia is formally defined as a pulse rate of less than 60 beats per minute. However, in hospital settings, a pulse rate above 50 rarely leads to any clinical consequences. Therefore, in the hospital setting, I redefine bradycardia as a pulse rate of less than 50.
Don’t hold medications unless HR < 50, it’s ok to give medications like beta blockers, non-dihydropyridine calcium channel blockers, and clonidine as long as the pulse rate is ≥ 50.
Detection
Bradycardia in the hospital setting is picked during a vital sign check, on telemetry, or a 12-lead EKG.
Information to get
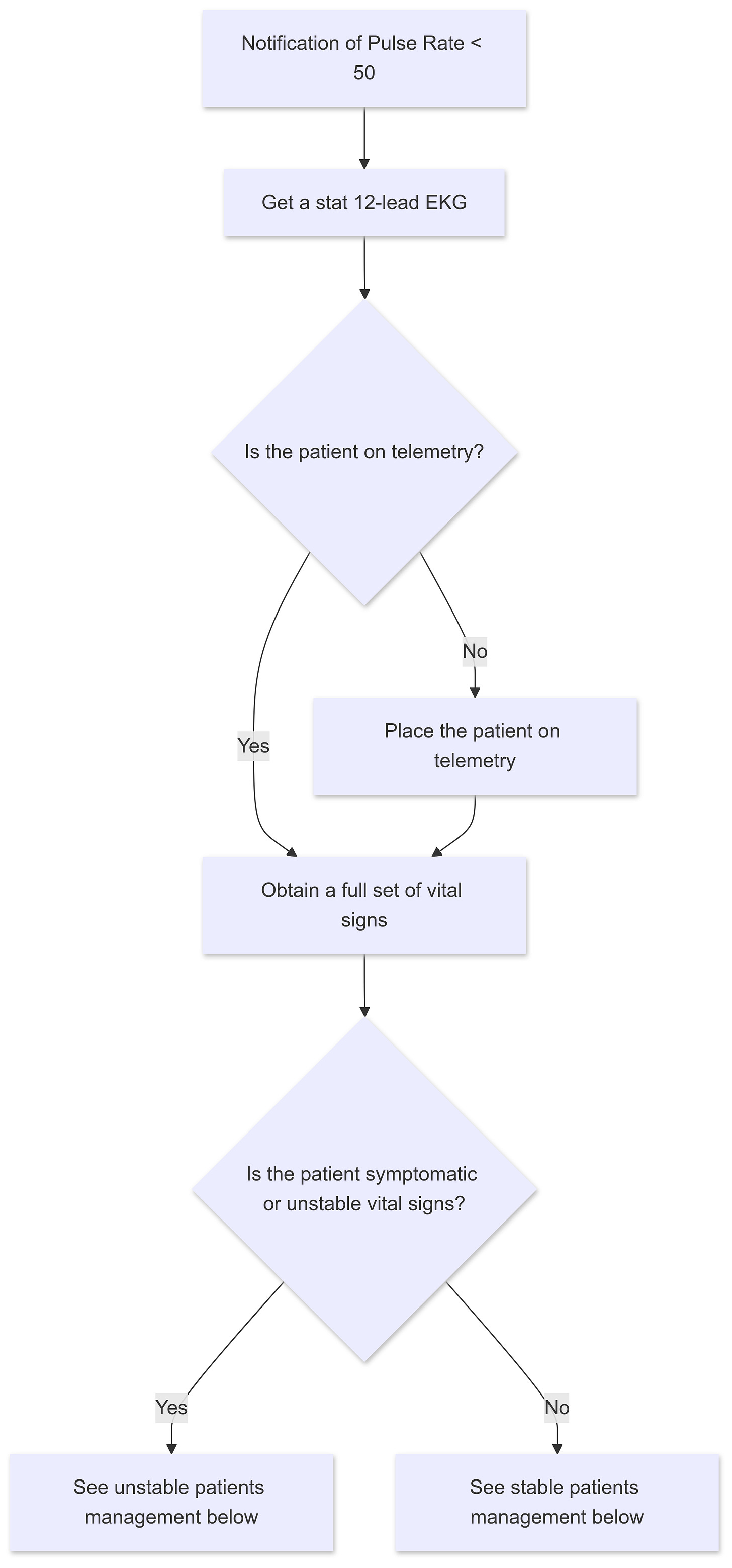
- Whenever I get notified of a pulse rate below 50:
- Get a stat 12-lead EKG, A 12-lead EKG is the first step anytime you are informed about an event on telemetry.
- Place the patient on telemetry if they are not on telemetry yet.
- Is the patient symptomatic? Bradycardia may cause symptoms like dizziness, lightheadedness, syncope, chest pain, shortness of breath, and altered mental status.
- Obtain a full set of vital signs.
Management
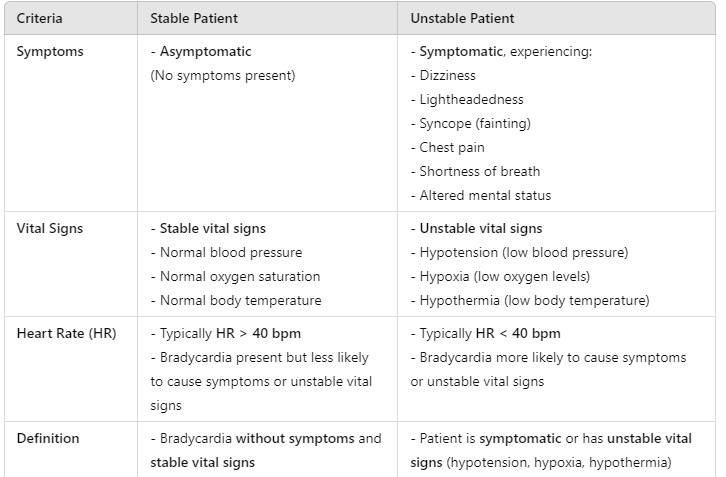
Unstable patients vs stable patients
- The patient is considered unstable if symptomatic or has unstable vital signs (hypotension, hypoxia, and/or hypothermia).
- Unstable vital signs or symptomatic bradycardia occur mainly when the HR < 40, rarely if it’s > 40.
- Stable bradycardia = Asymptomatic + Stable vital signs.
Unstable patients
Unstable patients should be seen immediately!
- Follow the ABC (airway, breathing, circulation) protocol.
- Stabilize the patient by bringing the pulse rate to a safe level, the safe level is the pulse rate at which symptoms resolve and vital signs stabilize which is typically a pulse rate > 50.
- Activate the rapid response team, get the crash cart into the room, and place pacing pads on.
- If bradycardia is causing hypotension, administer 1-2 L of LR or NS and administer 1 mg of Atropine simultaneously. Atropine can be repeated every 3-5 minutes x 3 as needed.
- If hypotension persists, start dopamine infusion. Dopamine can be started simultaneously with IVF if hypotension is profound (SBP < 70/ DBP < 40).
- If HFrEF, start dobutamine infusion instead and avoid IVF.
Temporary pacing
- Temporary pacing is required when there’s no response to the initial treatment with fluid and atropine.
Some say we should start pacing simultaneously with IV fluid and atropine but I prefer to give the initial treatment some time to see if there is any response so we avoid transcutaneous pacing which requires sedation and can be very uncomfortable for the patient.
- Temporary transvenous pacing is the ideal temporary pacing mode but isn’t feasible at the bedside in emergencies! In most hospitals, it is placed by the cardiology team preferably in the cath lab.
- For transcutaneous pacing, inform the patient what to expect, ensure the patient is closely monitored, provide adequate analgesia and sedation, and set the pacing threshold ideally to keep HR > 50!
- Ketamine, Etomidate, Midazolam, and Fentanyl can all be used before starting transcutaneous pacing. For dosing please refer to your preferred drug reference book!
- Transition the patient into transvenous pacing ASAP! It’s more reliable and more comfortable for the patient.
- Transfer to ICU as soon as the patient is stable for the transfer.
- Consult cardiology stat.
- Make the patient NPO and provide strict bed rest to avoid falls.
- Discontinue any possible culprit medications.
The following medications are the most common causes of iatrogenic bradycardia in hospital settings: Beta-blockers, non-dihydropyridine calcium channel blockers, clonidine, Precedex, Digoxin, and amiodarone.
- Check for other causes of bradycardia like an acute MI, electrolyte disturbances,…etc.
- Continue temporary pacing, until bradycardia is resolved or a permanent pacemaker is implanted.
- The cardiology team is the one to decide if a permanent pacemaker is implanted.
Stable patients
- Get the following questions:
- Is the bradycardia an isolated brief episode, persistent, or intermittent?
- Does it happen during sleep only?
- Is it recurrent, what was the most severe episode?
- Occasional episodes of asymptomatic sinus bradycardia don’t require any further intervention.
- Sinus bradycardia during sleep is not uncommon, and the pulse rate can drop to the mid-thirties, it resolves quickly upon waking up and does not require further intervention or medication adjustment.
- Persistent asymptomatic sinus bradycardia likely represents the patient’s baseline as in athletes, where pulse rate is typically 40-50 and doesn’t require any further intervention.
- If the EKG or telemetry shows evidence of a high-grade AV block like Mobitz 2 second-degree AV block and third-degree AV block, transfer the patient to the ICU or a step-down unit as these patients may become unstable at any moment.
- The presence of LAFB (Left anterior fascicular block) in the setting of bradycardia is a sign of a potential high-grade AV block, you still can monitor them on the telemetry floor but keep a close eye on them.
- First-degree A-V block and Mobitz 1 second-degree AV block can be monitored on the telemetry floor.
- Medications known to cause bradycardia should be discontinued or adjusted if:
- The pulse rate is persistently < 50 and the bradycardia is persistent.
- High-grade AV block.
- Consult cardiology if a high-grade AV block or unexplained persistent sinus bradycardia is suspected.
- Check TSH and electrolytes to check for other reasons for asymptomatic bradycardia.
- As long as the patients remain asymptomatic and stable, a temporary pacemaker is not needed, the cardiology team will decide if a permanent pacemaker is to be placed in cases of high-grade AV block.
Pauses
- Sinus pause or arrest is characterized by temporary cessation of sinus node discharges.
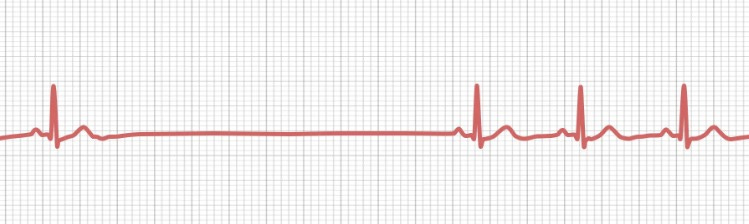
- When notified about a pause:
- Obtain a stat 12-lead EKG.
- Ask how long and frequent the pause is, and whether the patient is symptomatic.
- Sinus pauses less than 3 seconds usually need no investigation and may be seen in normal people; however, longer pauses ≥3 seconds require further investigation and treatment.
Most pauses are short and asymptomatic and require no further intervention.
- Recurrent long pauses need to be transferred to ICU/IMC. Very long and recurring pauses may require temporary pacing.
- Consult cardiology and discontinue all possible culprit medications.
- The cardiology team will decide if a permanent pacemaker is required.






Transfusion Medicine Made Simple: Essential Guide for Clinicians
Eight EKG patterns in acute MI we can’t afford to miss!
The top three antiemetics I rely on!
The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications