Introduction
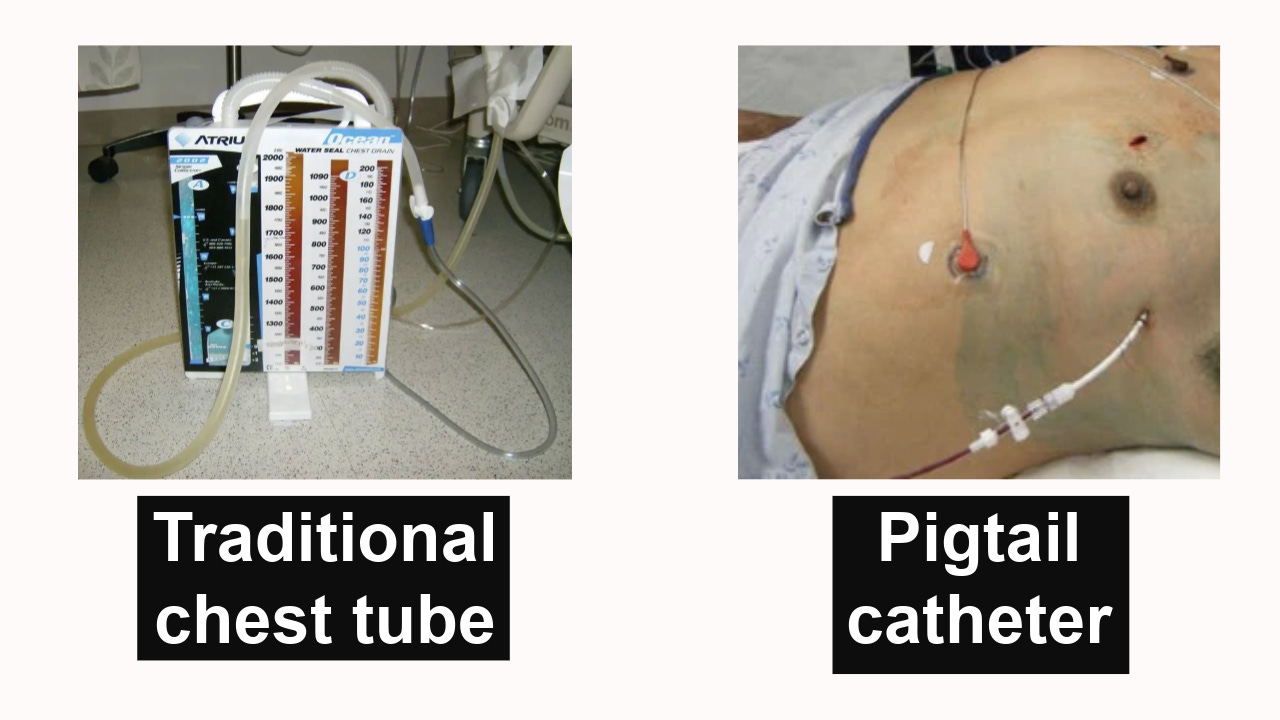
- A chest tube is a hollow, flexible tube that we place into the pleural space to drain air, blood, or fluid so the lung can re-expand.
- A pigtail catheter is simply a smaller, softer version of a chest tube, with a curled ‘pigtail’ tip.
- Both do the same job — removing air or fluid from around the lung — but the big difference is in size and invasiveness.
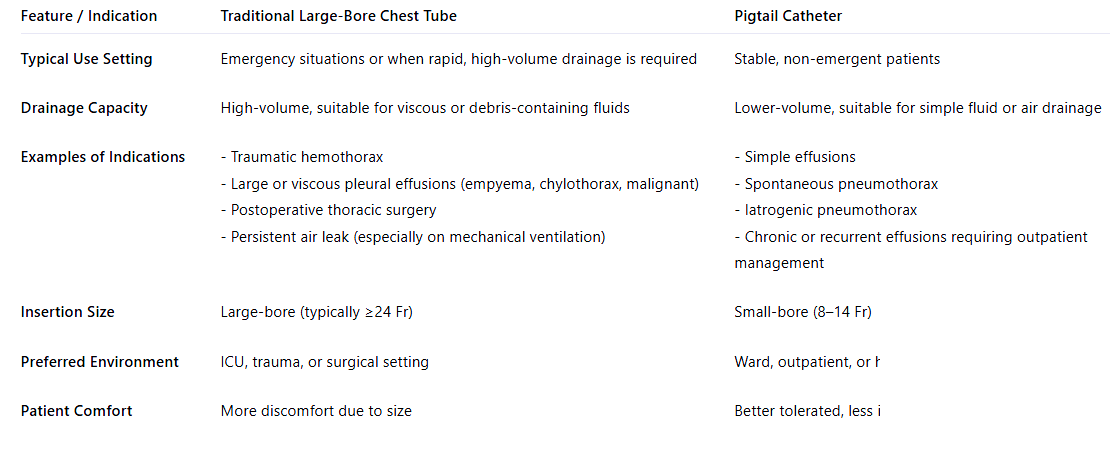
Indications
This table summarizes the indications of the traditional chest tube vs the pigtail catheter
The chest tube drainage unit
An adequate chest drainage system aims to:
- Remove pleural fluid and/or air.
- prevent their reflux into the pleural space.
- Restore negative pleural pressure (less than atmospheric pressure) to allow lung re-expansion.
To understand how the chest tube achieves that, we must understand the components of the chest tube drainage unit.
The one-bottle unit
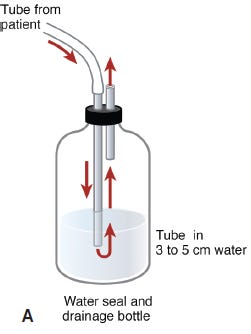
Back in the day, the chest tube unit was simply a tube connected to a bottle filled with saline/water and a one-way valve. While this works well for draining air, it doesn’t for fluid! If a pleural effusion is drained, the fluid level in the bottle will quickly increase, reducing the efficiency of removing additional fluid from the patient
The two-bottle unit
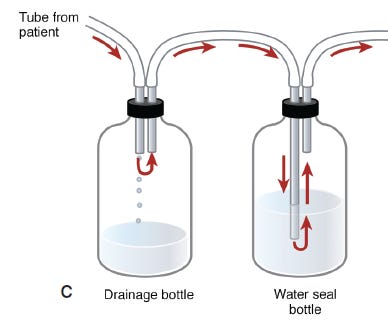
To solve this problem, a second water seal bottle was introduced! This leaves the first bottle for collection only and one for the water seal.
To understand the water seal, try blowing some air in a cup of water. You see all these bubbles; can you suck that air back? Of course, you can’t! The air gets sealed in the water.
The three-bottle system
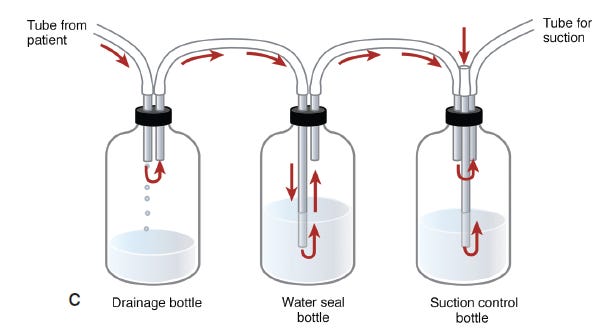
To improve drainage efficiency, a third bottle connected to external suction is added. a collection bottle, a water seal bottle, and a suction bottle.
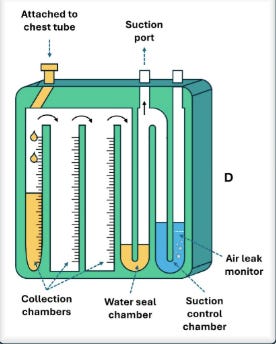
The modern chest tube unit
Nowadays, all these bottles/chambers are currently integrated into a single modern, multifunctional, easy-to-manage unit.
The tube itself comes in different sizes and shapes. They can be straight, angled, spiral, or coiled at the end (referred to as “pig-tail”).
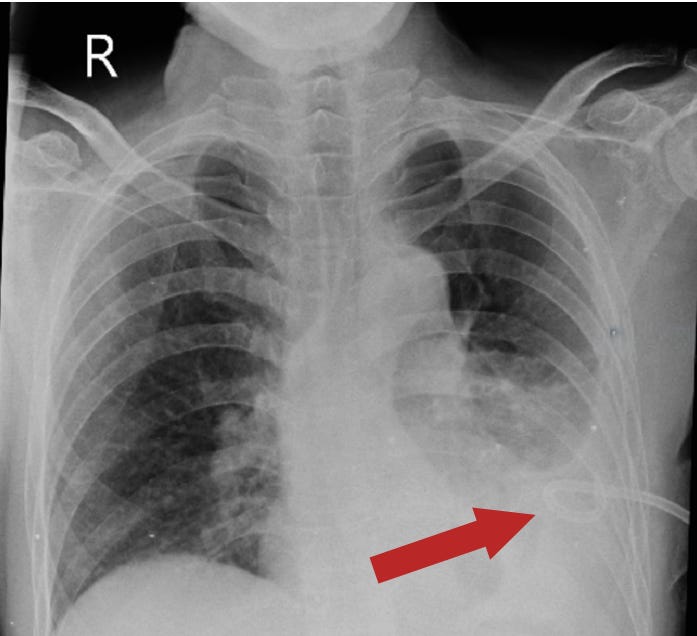
Confirmation of proper positioning with CXR
- Ideally, the tip of the chest tube should be positioned at the apex if inserted for pneumothorax, and at the base if inserted for fluid removal. Ensure the tip is not outside the pleural space or abutting the mediastinum.
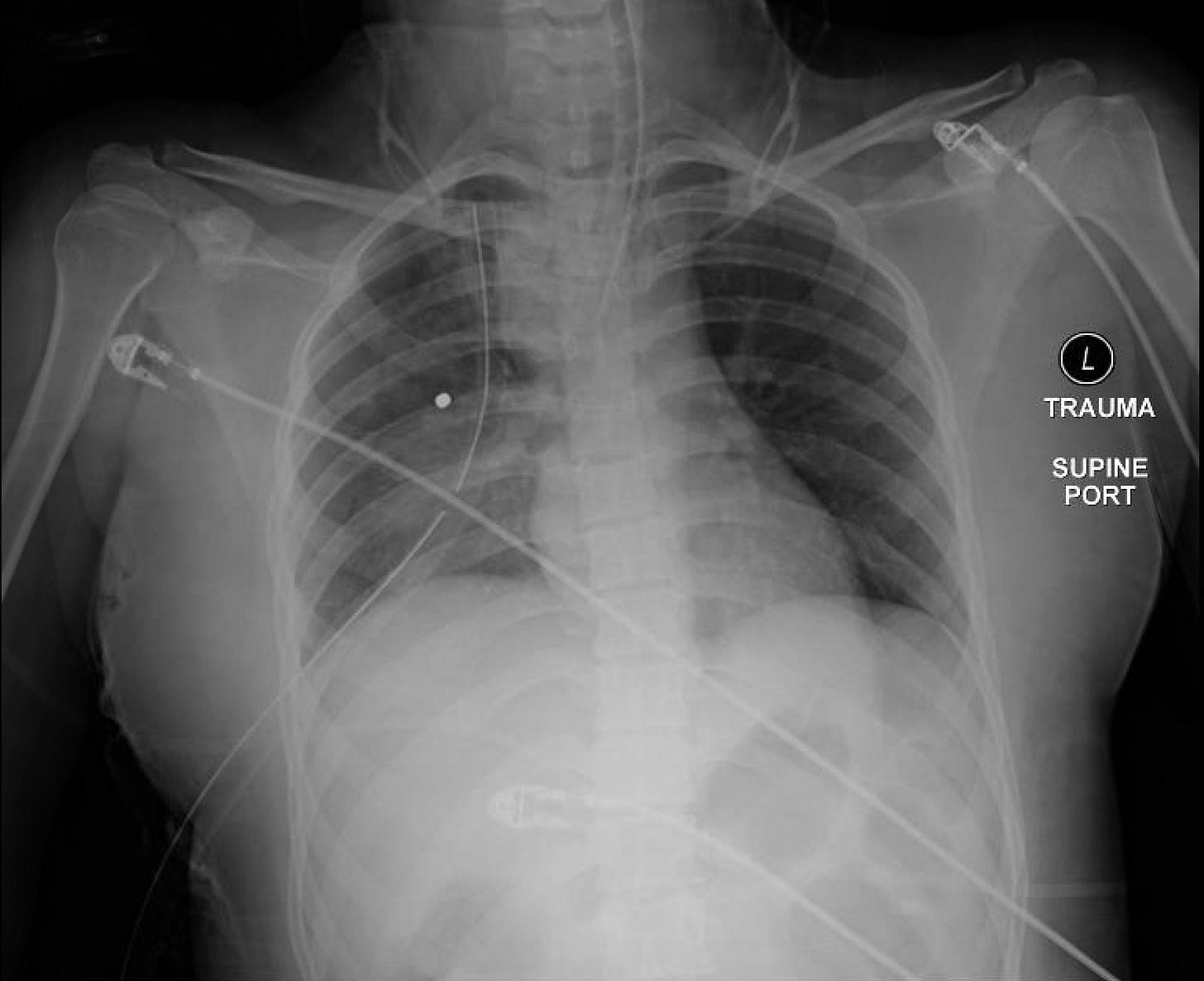
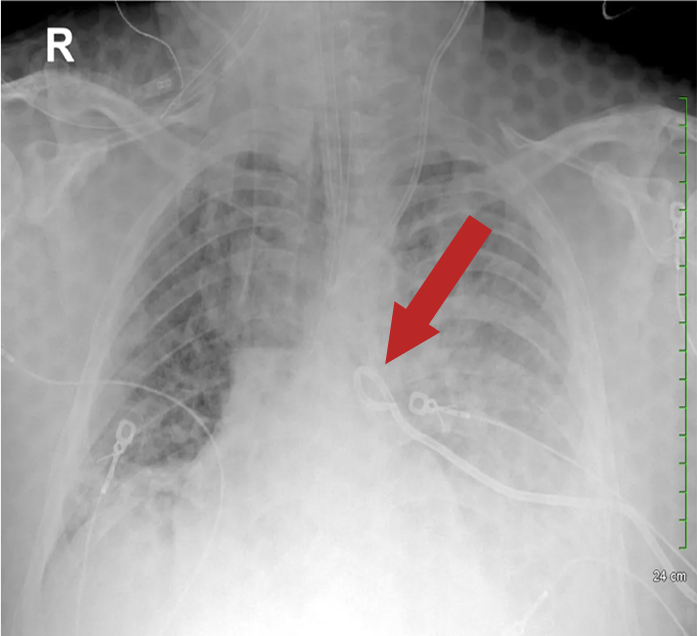

The fenestrations seen on chest tubes are these evenly spaced gaps (interruption marks) along the radiopaque stripe of the tube. The fenestrations should be inside the pleural space to allow effective drainage of air or fluid while reducing the risk of clogging or blockage. Multiple holes also distribute suction evenly, preventing tissue trauma and ensuring continuous tube function.
The daily bedside checks on patients with chest tubes
- Review the CXR first.
Although a daily CXR isn’t necessary in patients with chest tubes who are stable, it must be obtained if there is a change in the patient’s clinical status, after major adjustments, repositioning, or removal of the chest tube, or if there is a persistent air leak or fluid drainage.
- Assess the output in the collection compartment. Is it bloody or not? Is it increasing or decreasing?
- Check for tidaling! Tidaling is the rise and fall of fluid in the water seal chamber with breathing. Watch this YouTube video showing tidaling!
Tidaling tells you the chest tube is working and still in contact with the pleural space. If tidaling disappears, it means one of two things:
- The lung has fully re-expanded — which is good —
- The tube is blocked — which is bad —
If the patient’s breathing comfortably, chest X-ray shows full lung expansion, and there are no signs of distress — that’s good. But if the patient is short of breath, there’s new subcutaneous emphysema, or the tube is kinked or clogged — that’s bad, it means obstruction.
- Check for bubbling! Do you see any air bubbles in the air leak monitor? Check bubbles in the air leak monitor in this YouTube video:
Bubbling means air is still escaping. It could be from an ongoing air leak in the pleural space or a disconnection in the tubing outside the chest.
Never clamp a chest tube if bubbling is present, please! If you do, tension pneumothorax can develop quickly.
- Check the dressing and assess the tube integrity from the dressing to the tube unit, particularly if you see a continuous bubbling in the air leak monitor.
- Assess the Pain level! Chest tubes, especially large-bore ones, are painful, so please ensure adequate pain control.
- Ask them to ambulate. Chest tubes don’t mean they can’t be ambulated.
- Do they still need the chest tube?
Chest tube removal
The chest tube should only be removed by the team that placed and is actively managing it. Typically, the ICU, thoracic, cardiovascular, or trauma surgery team.
Removal is considered when:
- The active issue has been resolved, whether fluid or air.
- The lung has fully expanded.
- The patient is clinically stable.
For example, in cases of draining fluid, the amount in the collection compartment is consistently low; something like less than 20 cc/day for 1-2 days.
And for pneumothorax, you don’t see any air bubbles in the air leak monitor for 1-2 days, and the lung has fully expanded.
Typically chest tube is clamped for 12-24 hours (clamping deems the tube not functioning). If the patient’s conditions remained clinically stable with a stable CXR, then this means it’s time to remove the tube.
DO NOT CLAMP CHEST TUBE on your own unless you are part of the team who is actively managing it. DO NOT EVER CLAMP A TUBE IF YOU SEE AIR BUBBLES IN THE AIR LEAK MONITOR!
Some patients may need the chest tube for weeks and months, like malignant effusions. In such a case, a traditional chest tube can be replaced with a pigtail catheter to go home with.
Pitfalls & Warnings
- Don’t connect the chest tube to suction immediately after insertion to reduce the risk of re-expansion pulmonary edema. Re-expansion pulmonary edema is a non-cardiogenic edema that happens when a lung that’s been collapsed for days is rapidly reinflated — the fragile capillaries leak, flooding the alveoli. Management is supportive with oxygen, noninvasive ventilation, and cautious fluids. The real key is prevention: never drain too much, too fast.
Diuretics may worsen hypovolemia and are not recommended. The re-expansion pulmonary a non-cardiogenic edema driven by increased capillary permeability from reperfusion injury, not by fluid overload
- Watch for a blocked/clogged tube (no drainage but effusion enlarging). Sometimes, a thrombolytic is used for clogged tubes!
- Correct any tube kinking or dislodgment.






The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications
Chest Tubes & Pigtails: 5 Must-Know Tips for ICU Rotation
Mechanical Ventilation Made Simple: 9 Concepts Every Non-ICU Doc Should Know
NG Tube : 5 Things to know before your hospital rotations
Master ICU Vasopressor Management: 8 Shock Resuscitation Tips