In this post, I will share when to use them, how to use them, what to monitor, and their alternatives:
(1) IV Vancomycin
- In the ICU, I reach for IV vancomycin when MRSA or resistant gram-positives are a concern — like sepsis of unknown source, ventilator pneumonia, line infections, or resistant Strep pneumo meningitis. It’s my go-to until cultures guide me otherwise, with close drug monitoring and quick de-escalation when I can.
- The initial loading dose is 20-35 mg/kg, based on actual body weight, and should not exceed 3,000 mg. So, for a 70 kg patient, it’s roughly 1.5-2 gm. Do not renally adjust for the loading dose!
- Subsequent dosing is guided by the area under the concentration-time curve to minimum inhibitory concentration ratio (AUC/MIC), not by trough-only monitoring. Fortunately, our pharmacists take care of that.

- Vancomycin can cause nephrotoxicity and agranulocytosis, which is why we monitor kidney function and CBC while on IV vancomycin.
- Vancomycin infusion reaction (previously “Red man syndrome”) occurs with IV administration. It’s a side effect, not a true allergy. Manage by slowing the infusion rate to 50% or 10 mg/min (whichever is slower). Diphenhydramine plus famotidine effectively relieves symptoms. Stop infusion only for hypotension, chest pain, dyspnea, or muscle spasms; restart at reduced rate when resolved.
- Remember that Oral vancomycin is solely used for C. diff treatment.
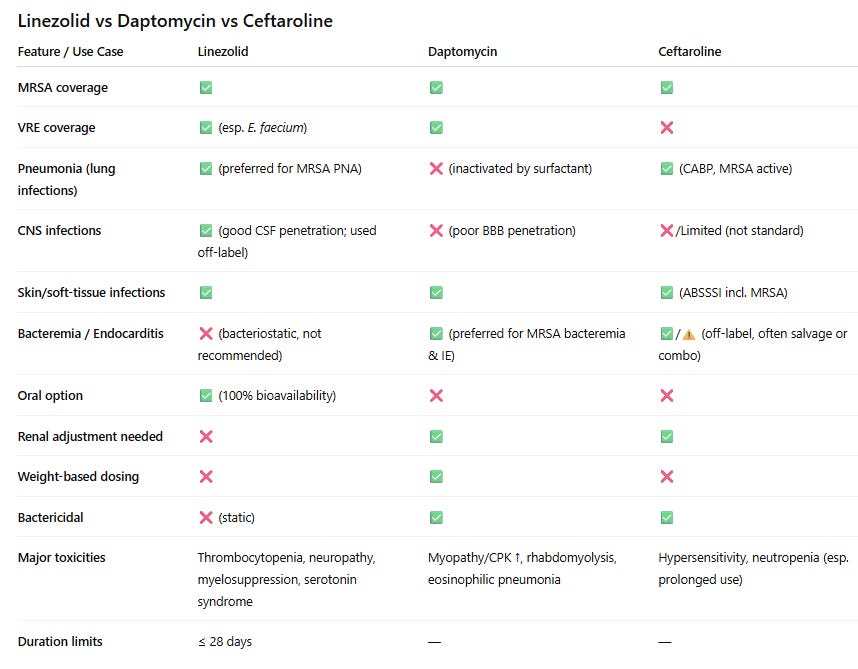
If I can’t use IV vancomycin because of allergy or toxicity, Linezolid and daptomycin are the main alternatives, and the source of infection dictates which is better to pick:
- Linezolid → preferred for lung, CNS, and skin/soft tissue infections. Easy, weight-independent dosing, 100% oral bioavailability, and safe in renal failure. But it’s bacteriostatic, not ideal for bacteremia, and can’t be combined with serotonergic drugs due to serotonin syndrome risk. Limit use to ≤28 days because of thrombocytopenia, neuropathy, and myelosuppression.
- Daptomycin → preferred for bloodstream infections, endocarditis, and other deep-seated infections (MRSA or VRE). Bactericidal, but weight-based and requires renal adjustment. Never use it in pneumonia — it’s inactivated by surfactant. Rhabdomyolysis and eosinophilic pneumonia are potential serious side effects of daptomycin.
- Ceftaroline → the only β-lactam with MRSA activity. I reach for it when linezolid or daptomycin can’t be used or when the vancomycin MIC is elevated (≥2 μg/mL). It’s useful for pneumonia and bacteremia, but requires renal dose adjustment.
(2) Cefepime
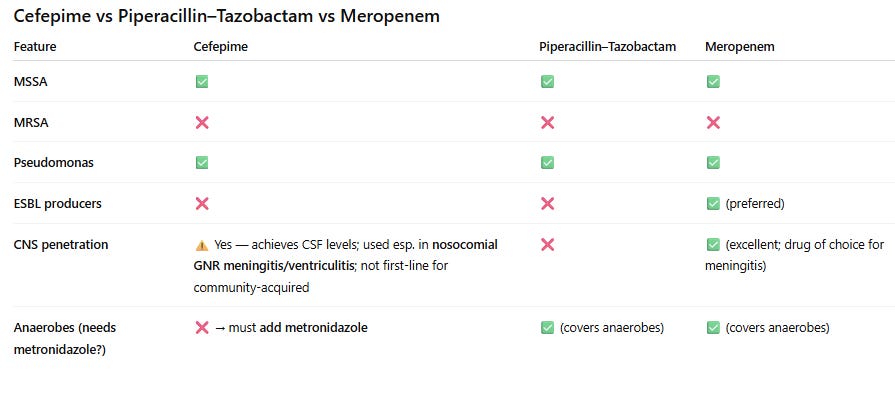
- I reach for cefepime when broad-spectrum coverage of Gram-negative and Gram-positive bacteria is required, such as in suspected hospital-acquired or ventilator-associated pneumonia, and sepsis of unknown source.
- That’s why you see quite often the combination of vancomycin and Cefepime in initial empiric treatment for severe infection and sepsis. Vancomycin to cover for MRSA and cefepime for the rest, including Pseudomonas. Cefepime lacks anaerobic coverage, and metronidazole should be added if anaerobic coverage is required.
- Cefepime has good CNS penetration and can be used to treat CNS infections.
- Cefepime isn’t effective against extended-spectrum beta-lactamase (ESBL) producing organisms, regardless of culture and susceptibility results. Use carbapenems instead for that.
- Dosing is 1-2 gm IV every 8-12 hours and should be adjusted to renal function.
- Monitor mental status to detect cefepime neurotoxicity early. Neurotoxicity in the form of encephalopathy, confusion, hallucinations, stupor, coma, aphasia, myoclonus, seizures, and nonconvulsive status epilepticus can all happen particularly with the use of high doses in patients with renal impairment.
- If penicillin allergy is reported in the patient’s chart, ask what kind of allergy. Cefepime should only be avoided in patients who report a history of immediate hypersensitivity reactions to penicillins (such as anaphylaxis, angioedema, or urticaria).
(3) Piperacillin/Tazobactam (Zosyn)
- In the ICU, I reach for Piperacillin/Tazobactam when broad-spectrum coverage of Gram-negativeincluding Pseudomonas, Gram-positive, and anaerobic bacteria is required (No need to add metronidazole).
- It was widely used in combination with vancomycin for the initial empiric antibiotic coverage for severe infections until it was found that this combination increases the risk of AKI! Since then, it has been largely replaced by cefepime.
- It has poor CNS penetration and shouldn’t be used for CNS infections.
- Dosing of (piperacillin and tazobactam) is dependent on the type and severity of infection being treated, and it requires renal dosing adjustment.
(4) Meropenem
- In the ICU, I reach for meropenem when ESBL-producing organisms are suspected, or when cefepime and piperacillin/tazobactam can’t be used due to a serious allergy.
- It covers Gram negatives, Gram positives, and anaerobes, and it has excellent CNS penetration, making it suitable for CNS infections.
- It has a very low cross reactivity with penicillin’s making it a great alternative in patients with serious penicillin allergy, even in those with a history of immediate hypersensitivity reactions (such as anaphylaxis, angioedema, or urticaria).
- Among carbapenems, ertapenem lacks pseudomonal coverage.
(5) Bactrim (Trimethoprim–sulfamethoxazole)
- The reason I include it here because it’s the antibiotic of choice to resort to when thinking about PJP pneumonia, Nocardia, and in the treatment of stenotrophomonas maltophilia, an opportunistic gram-negative bacillus that is a common culprit in hospital-acquired infections in critically ill patients.
- Dosing is weight-based. The IV preparation of Bactrim entails the use of a large volume of dextrose solution to mix with, so watch for the risk of hyponatremia.
- Renal adjustment is required; we need to closely monitor CBC, kidney function, and electrolytes as hyperkalemia, bone marrow suppression, and hyponatremia are all potential side effects of Bactrim.
- Allergy to nonantibiotic sulfas isn’t a contraindication to use sulfa antibiotics.
Conclusion
I know there are many other important antibiotics I didn’t cover today. I wanted to keep this post focused and concise. If you’d like a bit deeper practical dive into the antibiotics we use most often in clinical practice, check out my eBook: Antibiotics in Real-Life Clinical Practice: A Pocket Guide for Residents, Hospitalists, Internists, Nurse Practitioners, and Physician Assistants. Check it out here






The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications
Chest Tubes & Pigtails: 5 Must-Know Tips for ICU Rotation
Mechanical Ventilation Made Simple: 9 Concepts Every Non-ICU Doc Should Know
NG Tube : 5 Things to know before your hospital rotations
Master ICU Vasopressor Management: 8 Shock Resuscitation Tips