Introduction
Any specific antibiotic works against gram-positive, gram-negative, or anaerobes or a combination of them. This means we have three spectrums: anti-gram-positive, anti-gram-negative, and anti-anaerobic.
In clinical practice, it’s most effective to classify antibiotics from two perspectives: their spectrum of activity and the specific bacteria they target.
Spectrum classification
Single-spectrum antibiotics
- Pure anti-anaerobes: Metronidazole is the only pure anti-anaerobes antibiotic, it has zero gram-positive or gram-negative coverage.
- Pure anti-gram positive coverage without any clinically significant anti-gram-negative or anti-anaerobic activity: Vancomycin, Linezolid, Daptomycin, Oritavancin, Dicloxacillin, Cloxacillin, Oxacillin, and Nafcillin.
- Pure anti-gram negative coverage: This group includes Aztreonam, polymyxin B, and colistin. It has pure anti-gram-negative activity but no clinically significant anti-gram-positive or anti-anaerobic activity.
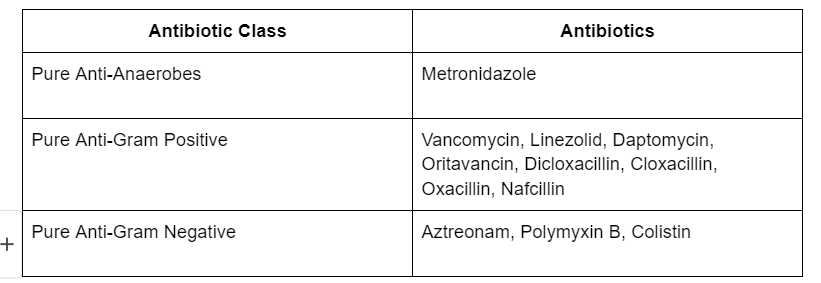
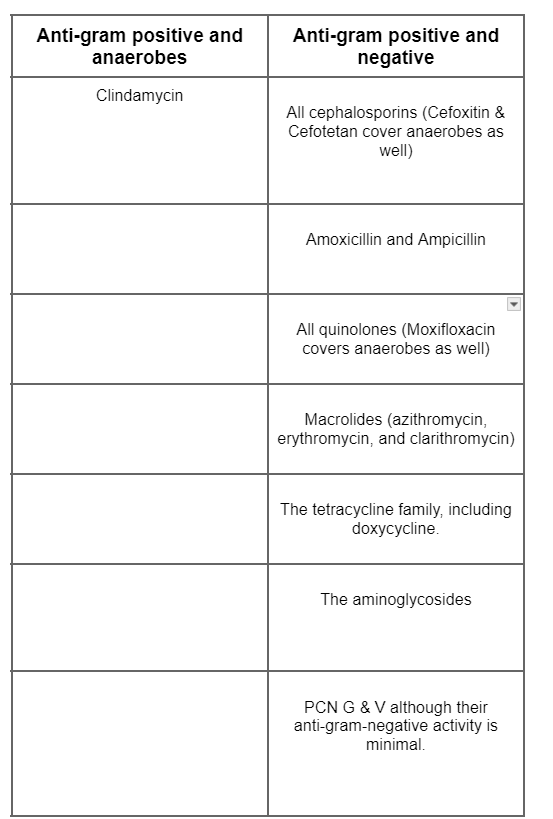
Double-spectrum antibiotics
- Anti-gram-positive & anti-anaerobes w/o any gram-negative coverage: Clindamycin is the only one in this category.
- Anti-gram-positive & anti-gram-negative: This is the most common group of antibiotics and includes the following:
- All cephalosporins except cefoxitin and cefotetan which are active against anaerobes as well.
- Amoxicillin and Ampicillin from the broad-spectrum penicillins.
- All quinolones except moxifloxacin which is active against anaerobes as well.
- Macrolides (azithromycin, erythromycin, and clarithromycin).
- The tetracycline family, including doxycycline.
- The aminoglycosides (gentamycin, tobramycin, and amikacin), remember that aminoglycosides are mainly used synergistically with other antibiotics
- PCN G & V although their anti-gram-negative activity is minimal.
Double-spectrum antibiotics
Triple-spectrum coverage (active against gram-positive, gram-negative, and anaerobes)
- The Carbapenems family.
- The extended-spectrum penicillins family (piperacillin/tazobactam, ampicillin/sulbactam, amoxicillin/clavulanic acid).
- Cefoxitin & Cefotetan form the cephalosporins.
- Moxifloxacin from the quinolones.
- Tigecycline ( The only one in this group that’s active against MRSA).
Anti-specific bacteria antibiotics
Anti-MRSA
The following antibiotics are -to a variable degree- active against MRSA:
- IV vancomycin, oral vancomycin is solely used for the treatment of C. diff.
- linezolid (Oral & IV).
- daptomycin (IV only).
- ceftaroline (IV only).
- Tigecycline (IV only).
- Oritavancin (IV only).
- Active against community-acquired MRSA:
- Clindamycin (Oral & IV).
- Trimethoprim/sulphamethoxazole (Oral & IV).
- Doxycycline (Oral & IV).
Anti-MSSA (Methicillin-sensitive staph aureus)
- The most commonly used IV agents in clinical practice are Cefazoline and antistaphylococcal penicillins (Nafcillin, Oxacillin).
- For oral use cephalexin (Keflex), amoxicillin/clavulanic acid (augmentin), Cloxacillin, and Dicloxacillin.
- All anti-MRSA antibiotics are theoretically active here but we reserve them for PCN allergy patients, IV vancomycin, linezolid, clindamycin, and Bactrim are the ones to consider in such a case.
- Anti-MRSA antibiotics are not as effective as first-line anti-MSSA regimens, for example, IV vancomycin is less active than cefazoline or antistaphylococcal agents.
- Please, avoid using quinolones or ceftriaxone to treat MSSA as resistance can develop quickly.
Anti-enterococci (enterococcus fecalis and Enterococcus faecium)
- Ampicillin, ampicillin/sulbactam, Piperacillin/tazobactam, IV vancomycin, linezolid, and daptomycin are active against enterococci.
- Linezolid and Daptomycin can be used for VRE (Vancomycin resitant enterococci).
- Aminoglycoside or ceftriaxone can be used synergistically with ampicillin in enterococcal bacteremia but never alone.
Antipseudomonal agents
- Piperacillin/tazobactam from the extended-spectrum PCN.
- The carbapenems family except for ertapenem which is not active against pseudomonas.
- Cefepime and ceftazidime from the cephalosporin family.
- Ciprofloxacin and levofloxacin from the quinolones, and are the only available oral agents to treat pseudomonas.
- Aztreonam.
- Aminoglycosides, remember Aminoglycosides are used synergistically with other antibiotics.
- Ceftazidime/avibactam, Polymixin B and colistin are reserved for panresistant pseudomonas.
Anti-ESBL-producing bacteria
- ESBL(extended-spectrum beta-lactamase)-producing bacteria are gram-negative bacteria specifically E.coli and Klebsiella pneumonia.
- Carbapenems family is the antibiotic of choice.
- If carbapenem can’t be used for any reason, high doses of cefepime can be used as a second-line agent, don’t pick piperacillin/tazobactam (zosyn) or other cephalosporins even if the culture says it’s sensitive to, they aren’t reliable!
Miscellaneous
- Stenotrophomonas maltophilia: Trimethoprim/sulfamethoxazole (Bactrim) is the drug of choice, and quinolones are the second line.
- PJP (Pneumocystis jirovecii): Trimethoprim/sulfamethoxazole (Bactrim) is the drug of choice.
- C. diff: Fidaxomicin, oral Vancomycin, and Metronidazole (Oral and IV).
- Legionella, mycoplasma PNA, and chlamydia PNA: These bacteria don’t gram stain well mainly M.PNA and C.PNA, respiratory quinolones or azithromycin are the drugs of choice ( Ciprofloxacin isn’t a respiratory quinolone and shouldn’t be used in CAP treatment).
Wrap up
- Quinolones are the only oral agents available to treat pseudomonas.
- Metronidazole is a pure anti-anaerobes.
- All cephalosporins cover the gram-positive and gram-negative bacteria but lack anaerobic coverage except cefoxitin and cefotetan.
- Vancomycin is less effective than cefazoline in treating MSSA.
- Ertapenem is the only carbapenem that doesn’t cover pseudomonas.
- Don’t use ceftriaxone or levofloxacin to treat staph.
- Carbapenems are the drug of choice to treat ESBL-producing bacteria.
- Moxifloxacin is the only quinolone that has anaerobic coverage.






Central Venous Access: What You Need to Know Before Starting Inpatient Rotations
10 Medications You Must Master Before Your ICU Rotation
Positive troponins! MI or not?
Comprehensive Guide to Antibiotic Spectrum: Gram-Positive, Gram-Negative, and Anaerobic Coverage