Clinical relevance
- The four clinical scenarios in which you will encounter metabolic alkalosis the most are:
- Volume depletion, particularly, those due to vomiting or over-diuresis.
- Volume overload, particularly, those who are being actively diuresed.
- Chronic respiratory acidosis when CO2 is acutely reduced with BIPAP or mechanical ventilation (post hypercapnic alkalosis) if associated with with stimulant for HCO3 gain typically volume depletion.
- Iatrogenic from bicarbonate therapy oral or IV.
Pathophysiology
- For metabolic alkalosis to develop, two conditions must present:
- HCO3 gain (direct & indirect).
- Sustained HCO3 renal absorption (Direct & indirect).
- Almost all of the filtered HCO3 is reabsorbed in the proximal tubule. This process is very effective to keep the HCO3 22-26, any HCO3 above this concentration will be expelled in the urine returning the HCO3 level to normal.
- The following factors increase proximal tubule HCO3 reabsorption:
- Decreased intravascular volume whether from Volume depletion or volume overload.
- Severe hypokalemia
- Hypercapnia
Diagnosis
- Metabolic alkalosis is defined by a serum HCO3 > 26 in the abscess of a primary respiratory acidosis.
Treatment
- Stop the HCO3 gain (Treat the underlying cause).
- Excrete the excess HCO3.
- Discontinue any HCO3 or HCO3 precursors (Acetate or lactate) treatment
Hypokalemia
- Potassium must be repleted to correct metabolic alkalosis.
- Use KCL not K-acetate or lactate (Acetate and lactate are metabolized to HCO3 in the liver).
- Don’t forget to check Mg and replete if needed.
Volume depletion
- Volume depletion: Resuscitation with 0.9 NS (Saline responsive).
- Urine Cl < 10 (Unlike Na, Urine chloride isn’t affected by diuretics).
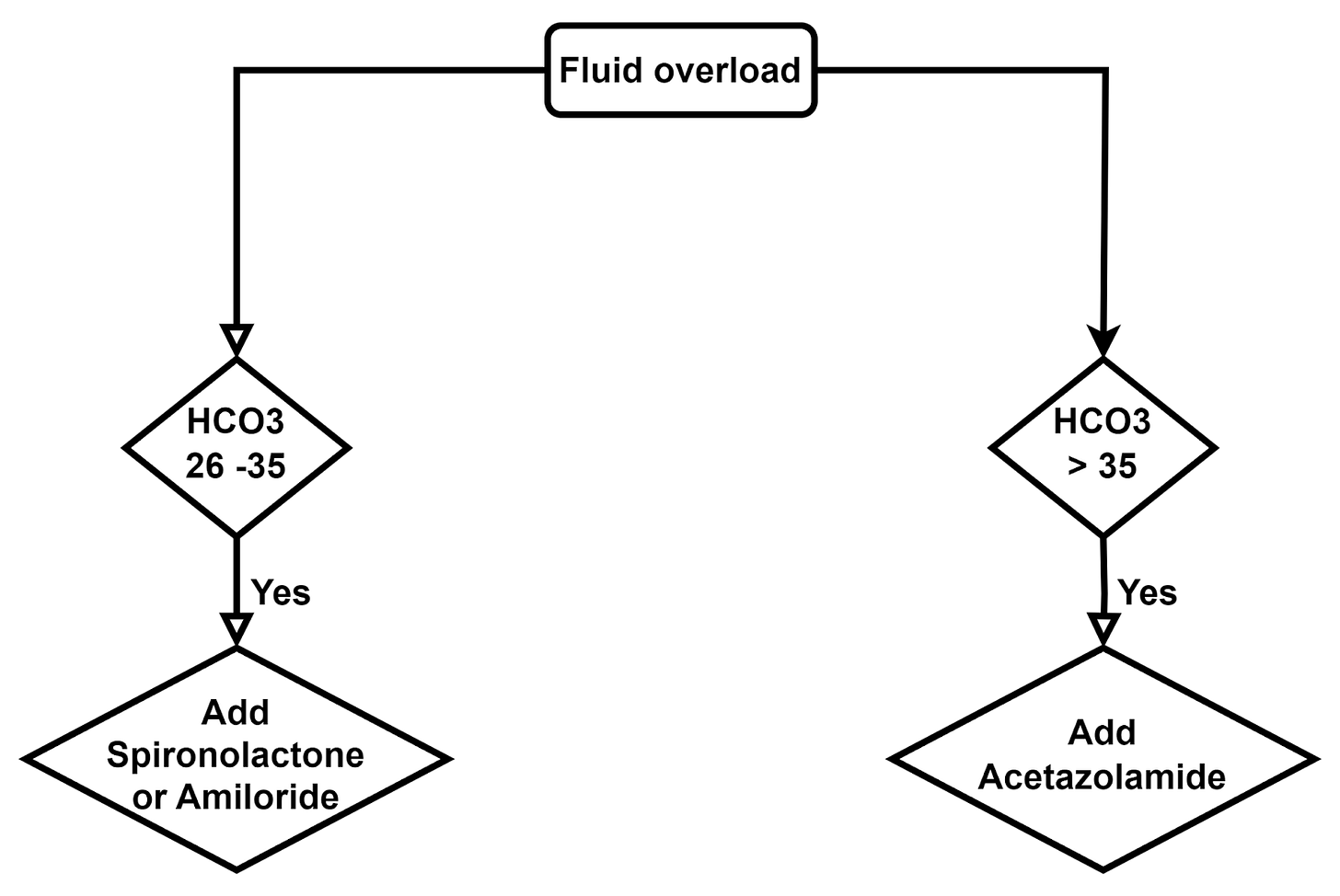
Volume overload
Diuretics
Acetazolamide: Strong HCO3 urinary loss, modest diuresis, exacerbate hypokalemia.
Spironolactone/Amiloride/Triamterene: Weak HCO3 urinary loss, weak diuresis, potassium-sparing.
Post hypercapnic
- Acute reduction of CO2 in patients with chronic CO2 retention.
- Most of these patients have volume depletion which sustains the elevated HCO3 and minimizes urinary excretion.
- Resuscitation with 0.9 NS.
- Replete K & Mg
Other causes of metabolic alkalosis
- Renal failure: rarely leads to metabolic alkalosis rather than acidosis → dialysis.
- Barter syndrome = loop diuretics → Potassium repletion and Amiloride.
- Gittleman syndrome = Thiazides diuretics → Potassium repletion and Amiloride.
- Cushing syndrome.
- Liddle syndrome → Potassium repletion and Amiloride/triamterene.
- Primary hyperaldosteronism.






Eight EKG patterns in acute MI we can’t afford to miss!
The top three antiemetics I rely on!
The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications
Chest Tubes & Pigtails: 5 Must-Know Tips for ICU Rotation