Introduction
- Volume overload = excess total body sodium.
- Loop diuretics are the mainstay treatment of volume overload.
- Diuresis means getting rid of excess sodium and water through the kidney.
Mechanism of action
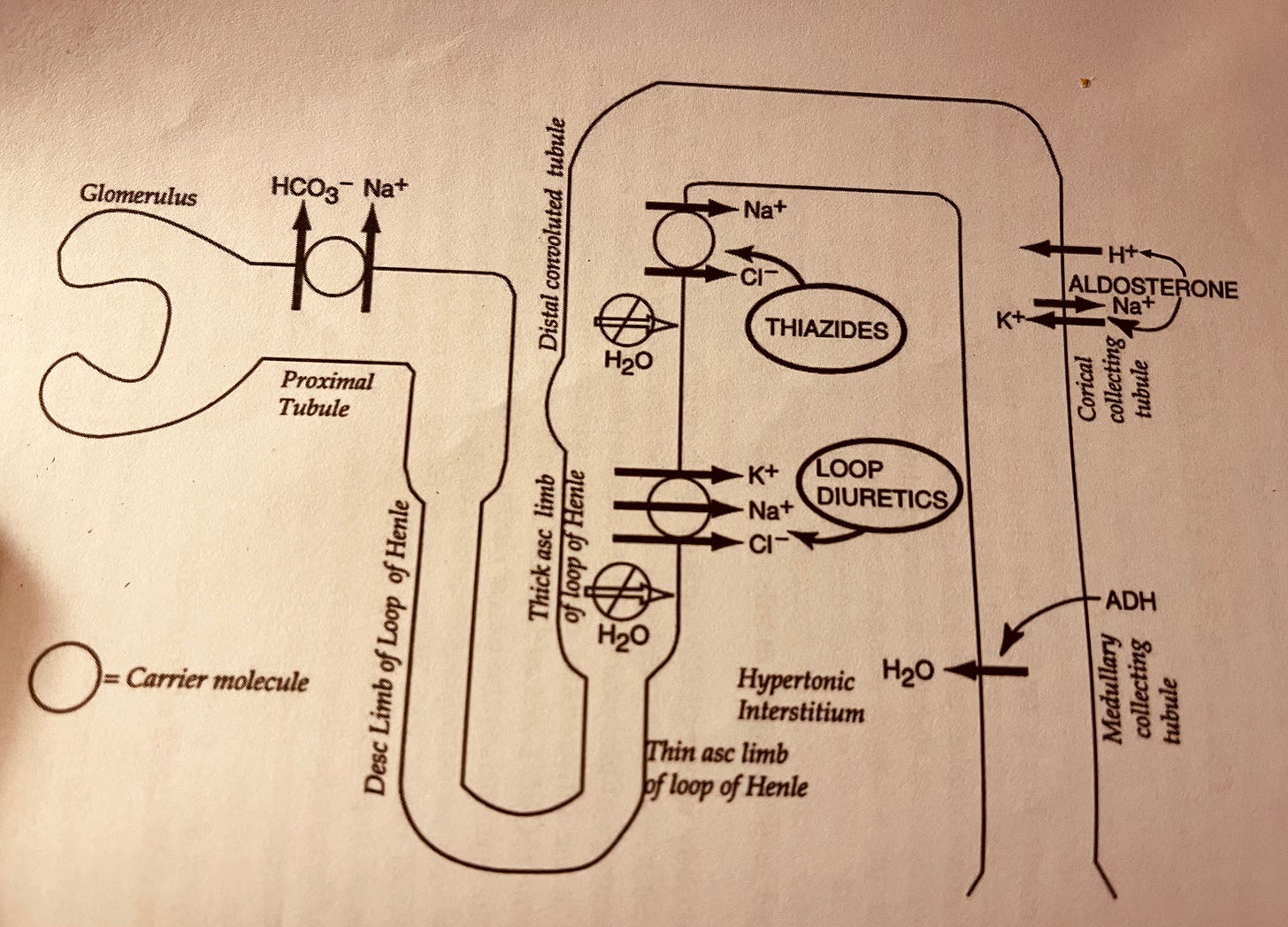
Loop diuretics:
- Are secreted in the proximal tubule rather than being filtered in the glomerulus as they are bound to protein
- Lead to the excretion of calcium as well.
- Produce diluted urine in contrast to thiazide diuretics.
- Lead to the excretion of 20-25% of the filtered sodium.
- Furosemide, Torsemide, and Bumetanide are sulfa-based, while Ethacrynic acid is the only non-sulfa loop diuretic (Should only be used if allergy to other loop diuretics.
- No cross-reactivity with sulfa antibiotics.
- The onset of action: 5 minutes for IV form, 30-60 minutes for oral form.
- Peak effect: 1-2 hours.
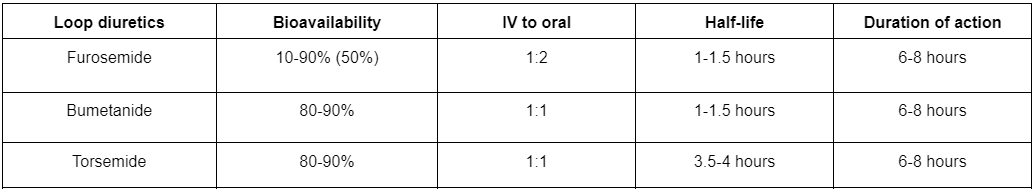
Loop diuretic dose conversion
- Furosemide: Torsemid 2 : 1.
- Furosemide to Bumetanide 20 : 1.
- Torsemide to Bumetanide 10 : 1.
- They are equally effective if given in equipotent doses.
Acute tolerance to loop diuretics
The action of loop diuretics lasts for the duration of action then quickly drops to almost zero, for example, if you give a dose of furosemide once daily you will get a diuretic effect for 6-8 hours (Furosemide duration of action) then quickly drops to almost zero for the rest of the day.
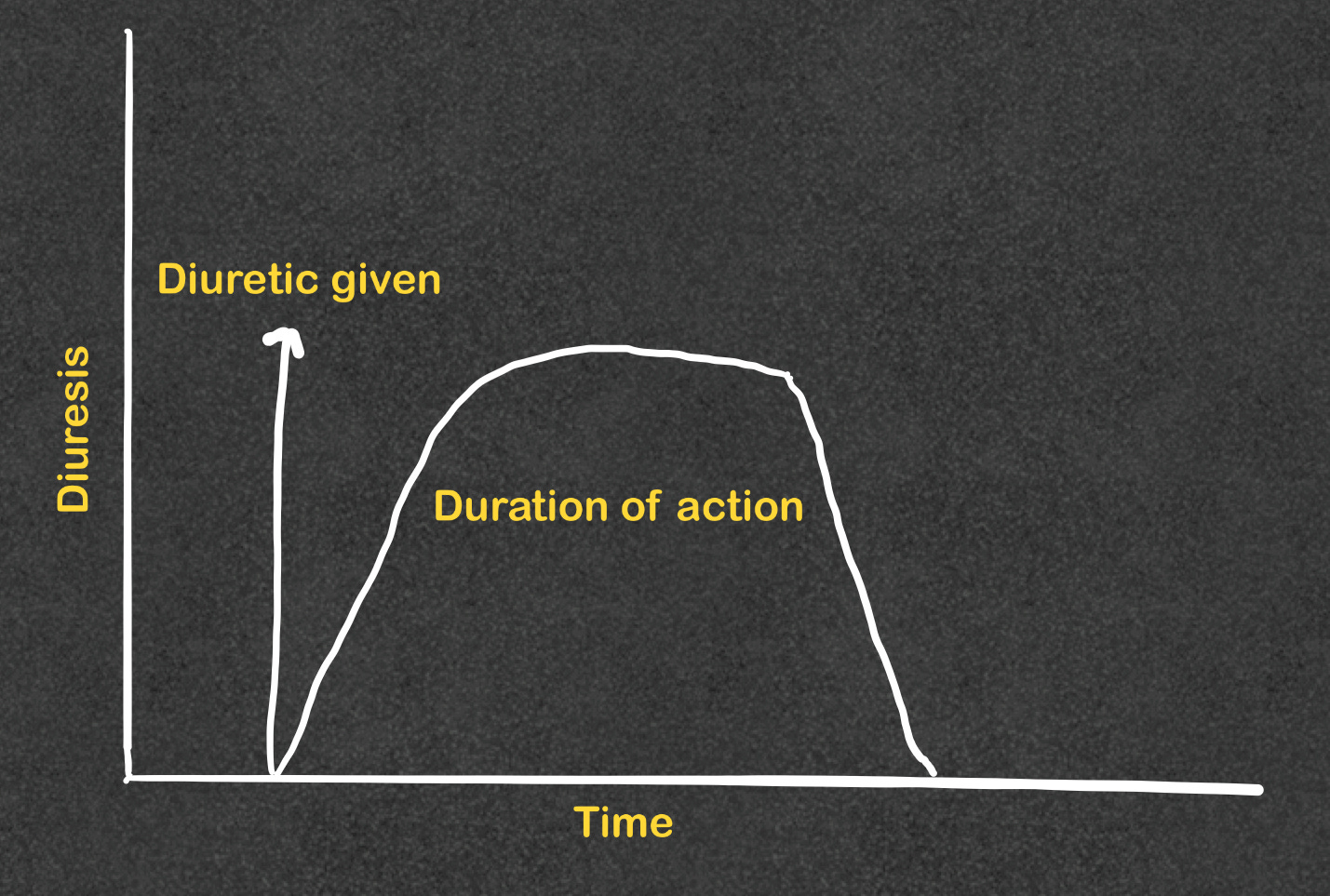
We overcome acute tolerance by:
- Adding a second and, if needed a third dose, the second and the third dose peak effect will be less than the first dose.
- Low sodium diet.
- Starting a continuous infusion of loop diuretics after a loading dose.
Chronic tolerance to loop diuretics
A patient on a fixed dose of loop diuretic and a fixed sodium intake, on average, after 1-2 weeks, Sodium excretion progressively decreases until it levels with sodium intake.
We overcome this by:
- Low sodium diet.
- Increasing the loop diuretic or frequency.
Loop diuretics administration
- Loop diuretics can be given as an intermittent bolus or a continuous infusion.
- Bolus: the loop diuretic works for the duration of action, and then the diuretic effect quickly drops to almost zero, to avoid this, a second and sometimes a third dose should be given.
- Continuous infusion (drip): the loop diuretic reaches peak effect after a loading dose and continues at the peak as long as the infusion runs.
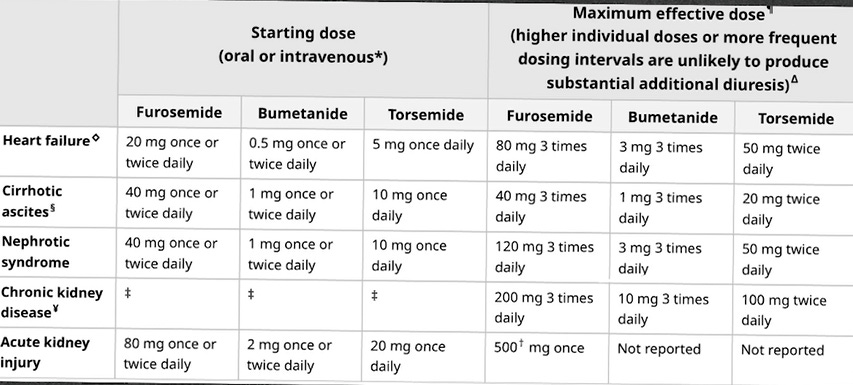
- Loop diuretics have a threshold dose; no diuretic effect is shown when the dose is lower than the threshold dose. The threshold dose of furosemide differs according to the clinical condition of the patient.
- Loop diuretics display dose-response curves, the higher the dose the more diuretic effect till we reach the maximum effective dose.
- Loop diuretics have a ceiling dose (maximum effective dose); this is the dose that shows the maximum sodium excretion, doses above the ceiling dose are only moderately effective.
-
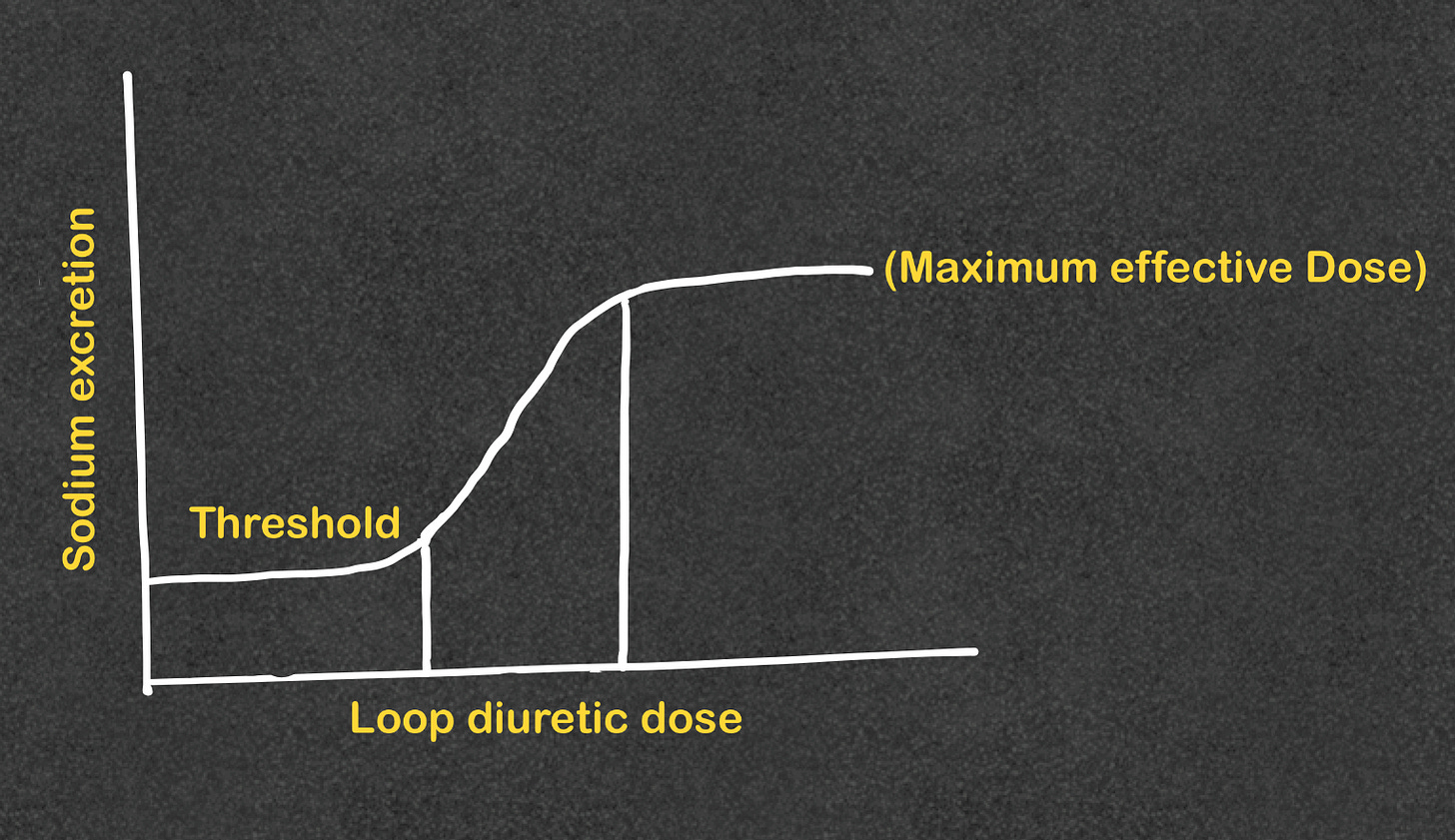
Threshold & maximum effective dose - Repeated infusions with the ceiling dose are more effective than increasing the dose of furosemide.
Maximum total daily dose and ototoxicity
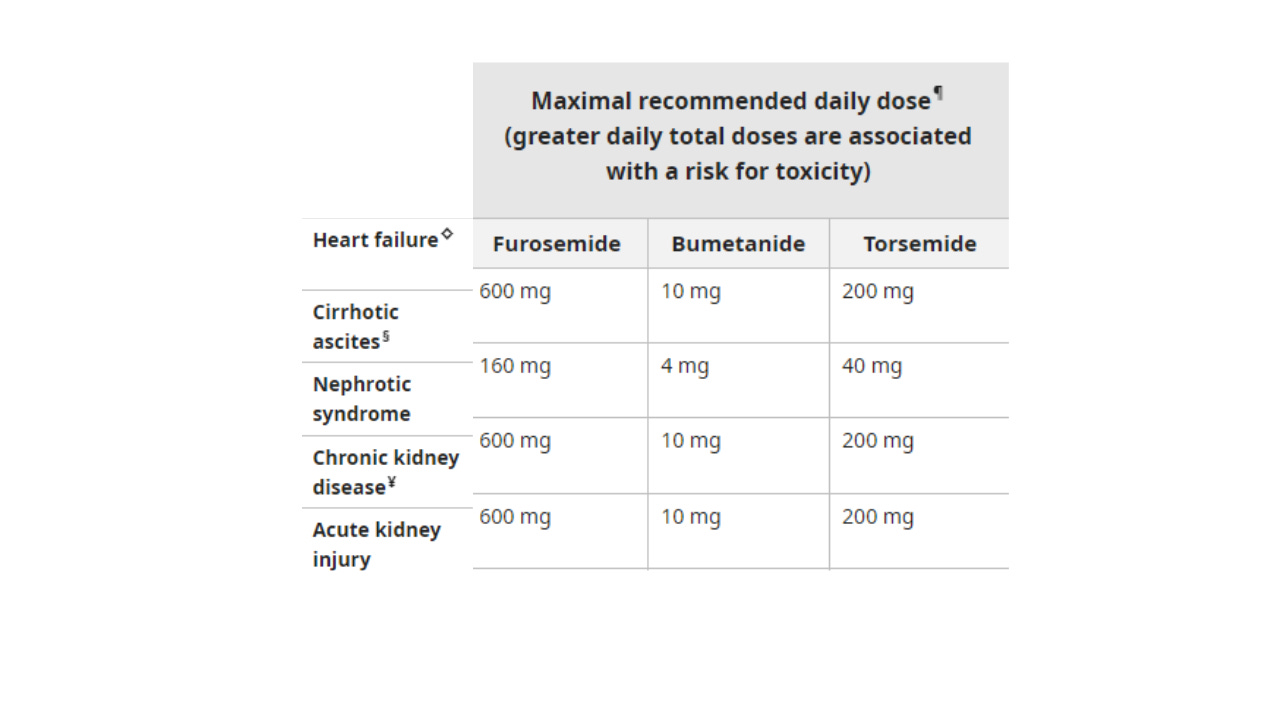
- Loop diuretic-induced ototoxicity can lead to transient (usually lasting 30 minutes to 24 hours) or permanent deafness.
- Ototoxicity primarily occurs with high-dose intravenous therapy (eg, furosemide doses above 240 mg/hour) or at lower doses in patients with kidney function impairment or concurrent use of other ototoxins such as aminoglycosides.
- Ethacrynic acid, which is rarely used, maybe more ototoxic in high doses than furosemide, torsemide, and bumetanide.
Measures in all patients with volume overload
- Low sodium diet.
- Daily weight (Weight is the most sensitive indicator of adequate diuresis).
- Strict I & Os (Foley’s catheter isn’t always necessary)
- Fluid restriction is only indicated if volume overload is associated with hyponatremia, restrict fluid to 800-1000 ml/day of all kinds of fluids.
Monitoring patients while on loop diuretics
- While on IV diuretics, obtain BMP or CMP, and Mg daily or every other day.
- Obtain daily weight as weight is the most sensitive way to check for effective diuresis (The patient should be weighed every morning before breakfast using the same weight scale).
- Strict I & O (achieve a daily negative fluid balance).
Worsening kidney functions while on diuretics
Over-diuresis
- Orthostatic hypotension
- Tachycardia
- Progressive elevation of BUN/CR + resolution of edema + negative fluid balance (worsening BUN/Cr by itself doesn’t automatically over diuresis as it can happen with worsening edema, see below).
- Discontinue diuretics, may need to start a resuscitative IV fluid.
Persistent edema
Consider adding 12.5-25 gm of albumin 15-20 minutes before administering Furosemide.
Titrating up diuretics
- Before titrating up diuretics:
- Check compliance with low sodium diet and diuretics.
- Verify if the dose is above the threshold dose.
- Increase the dose and/or frequency
- Increasing the dose to the maximum effective dose before increasing the frequency may be considered.
- Going above the maximum effective dose may be considered as this may increase the time the loop diuretic stays at the peak effect.
Diuretics in liver cirrhosis
- Low sodium diet + Spironolactone + Furosemide.
- Spironolactone is particularly helpful in edematous states caused or exacerbated by hyperaldosteronism, which is typical of the edema and ascites caused by cirrhosis.
- Spironolactone monotherapy is more effective than Furosemide monotherapy.
- Start at 40/100 mg (Remember the threshold dose) and increase by 40/100 to a maximum of 160/400 mg.
Volume overload and metabolic alkalosis
Loop diuretics + potassium-sparing diuretics.
Loop diuretics + Acetazolamide (if excessive diuresis is required), replete potassium aggressively to avoid profound hypokalemia.
Refractory edema
- Reinforce compliance with a low-sodium diet and diuretics.
- Titrate up to the maximum effective dose.
- Increase the frequency.
- Add Metolazone (Thiazide-related diuretic). Replete potassium aggressively.






The use of 3% NS in hyponatremia, when and how.
The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications
Chest Tubes & Pigtails: 5 Must-Know Tips for ICU Rotation
Mechanical Ventilation Made Simple: 9 Concepts Every Non-ICU Doc Should Know
NG Tube : 5 Things to know before your hospital rotations