Total serum calcium
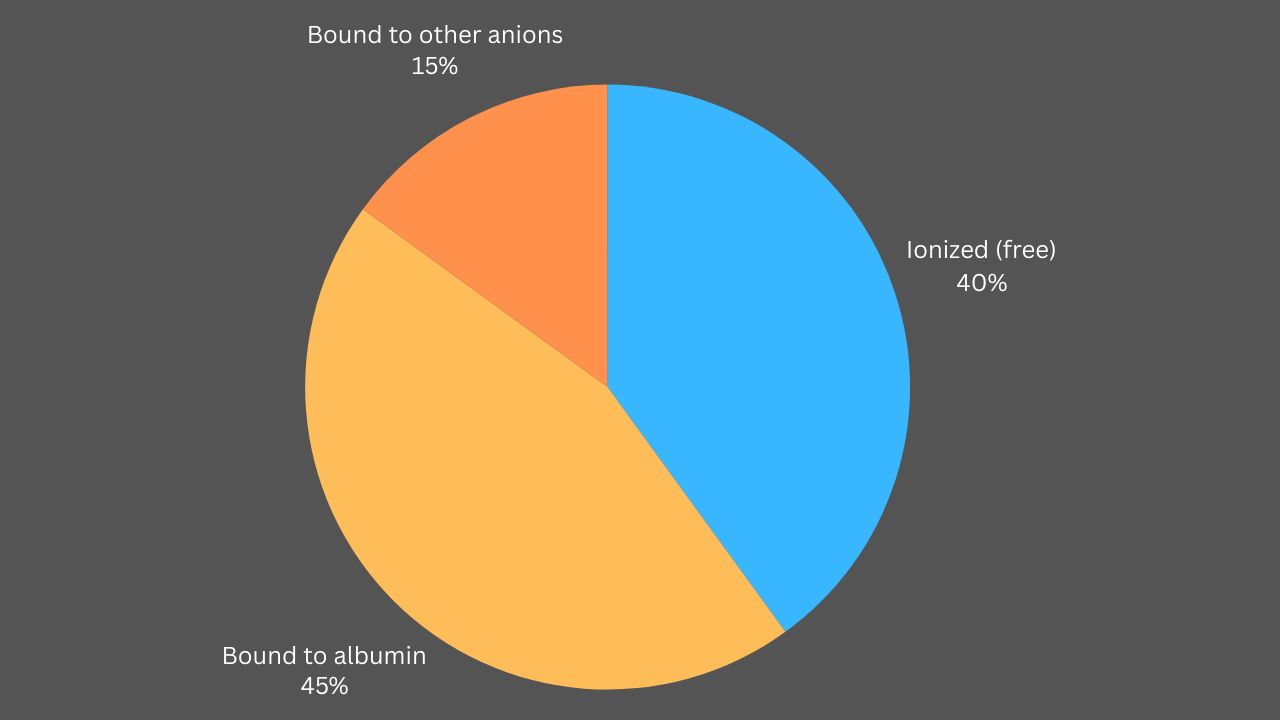
- The calcium level obtained on routine BMP/CMP is the total serum calcium.
- When the blood becomes too alkaline (alkalosis), more calcium gets tied up with albumin (a protein in your blood). This reduces the amount of free, or ionized, calcium
- Free or ionized calcium is the active form of calcium and is the one that gets regulated by PTH and vitamin D.
- Total calcium level doesn’t tell you much about free calcium levels.
- Total calcium levels can be falsely elevated or lowered by high or low albumin levels.
Diagnosis
Free/ionized calcium level:
- The gold standard to diagnose hypo/hypercalcemia.
- Expensive and not readily available.
- Normal reference values are assay-dependent and may vary from facility to facility (check your lab’s references).
- Alkalosis increases albumin-bound calcium and therefore reduces free/ionized calcium as in hyperventilation.
- PTH decreases albumin-bound calcium and therefore increases free/ionized calcium.
- Phosphorus binds calcium and therefore hyperphosphatemia decreases the ionized/free calcium as in CKD.
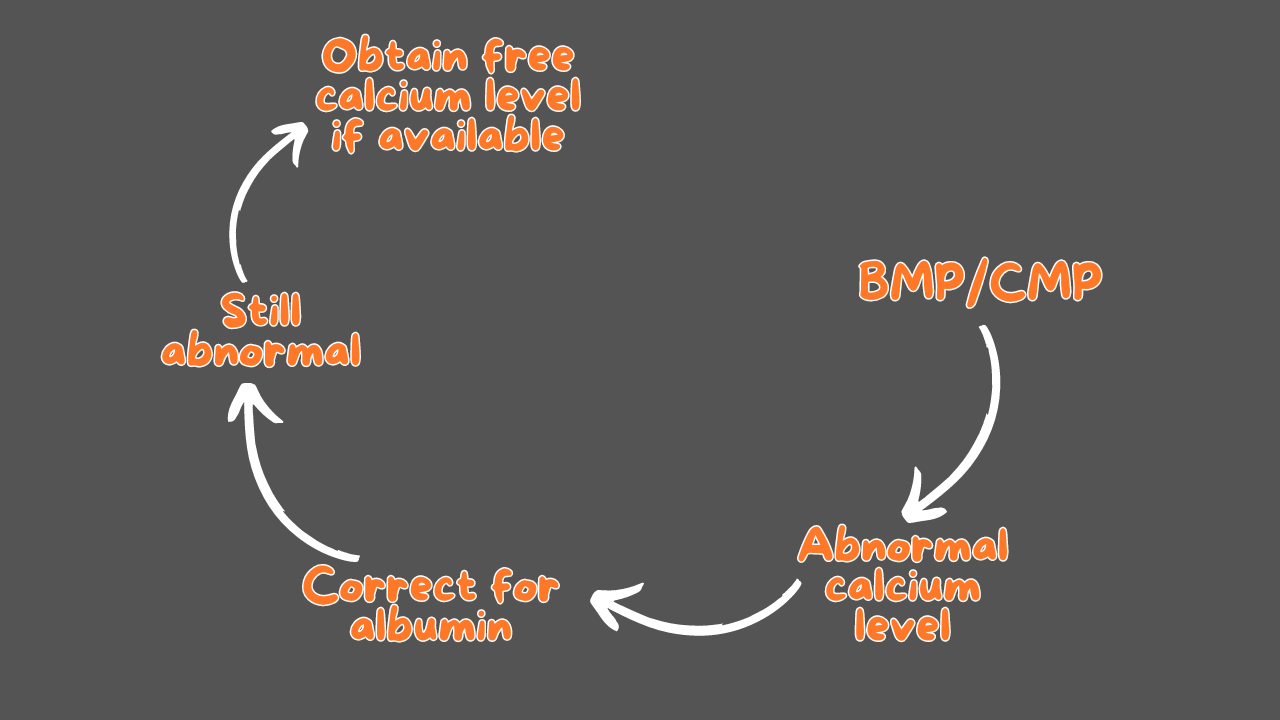
Total serum calcium level:
- This is the value obtained on routine BMP/CMP
- Correct total serum calcium level to albumin level whether albumin is high or low (no need if albumin is normal 4 gm/dl).
- Total serum calcium level changes by 0.8 mg/dl for each 1 gm change in albumin.
- Hypocalcemia = Ca level < 8 mg/dl (Corrected to albumin).
- Hypercalcemia = Ca level < 10 mg/dl (Corrected to albumin).
Confirm the diagnosis
Initial w/u
Check PTH and vitamin D levels.
Check Mg and phosphorus levels.
Check EKG (QTc).
Treatment
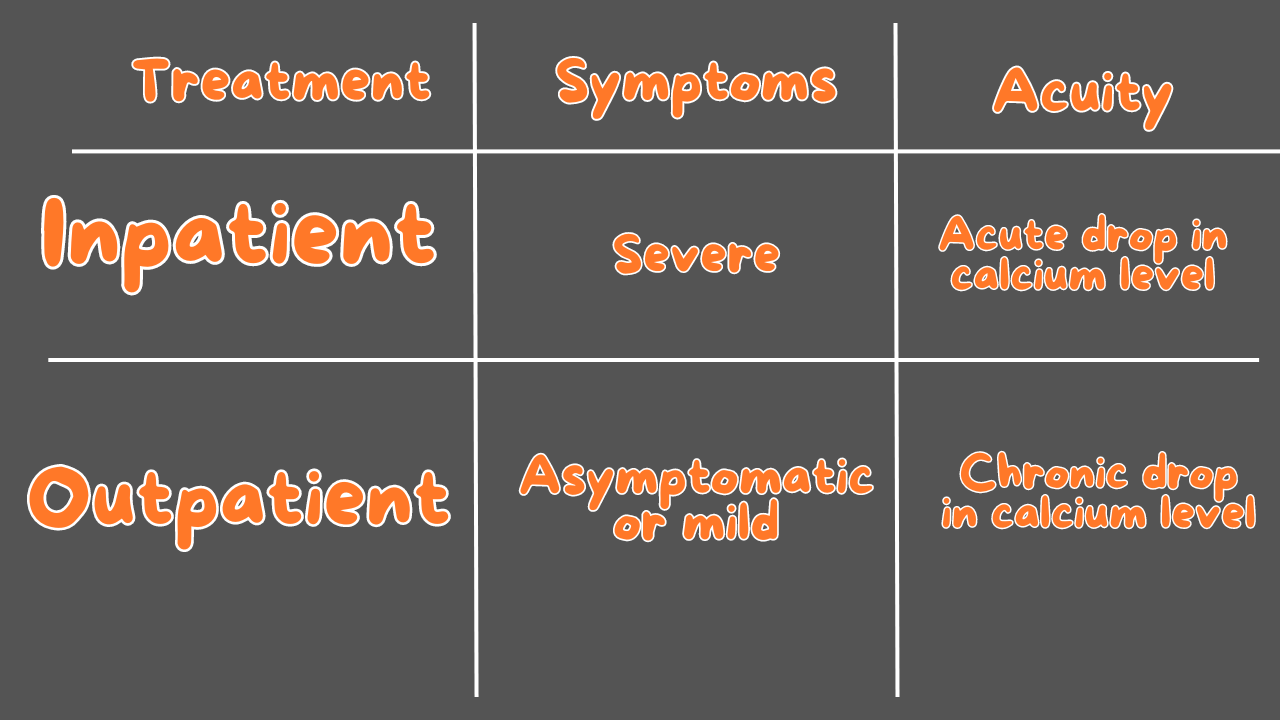
Acute hypocalcemia
- Acute drop in calcium level to < 7.5 mg /dl compared to a recent baseline.
- If no baseline is available, we consider it chronic.
Severe signs/symptoms
- Prolonged QTc.
- Chvostec’s/Trousseau’s sign.
- Seizures.
- Spasm:
- Carpopedal.
- Laryngeal.
- Bronchospasm.
- Irritability, anxiety, and depression.
Inpatient/urgent treatment
- A bolus or two of IV calcium will lead to a quick but temporary rise in serum calcium level enough to relieve or alleviate hypocalcemia-related symptoms.
- A slow calcium infusion or repeated boluses (at a slower rate) will lead to a more sustained rise in calcium levels.
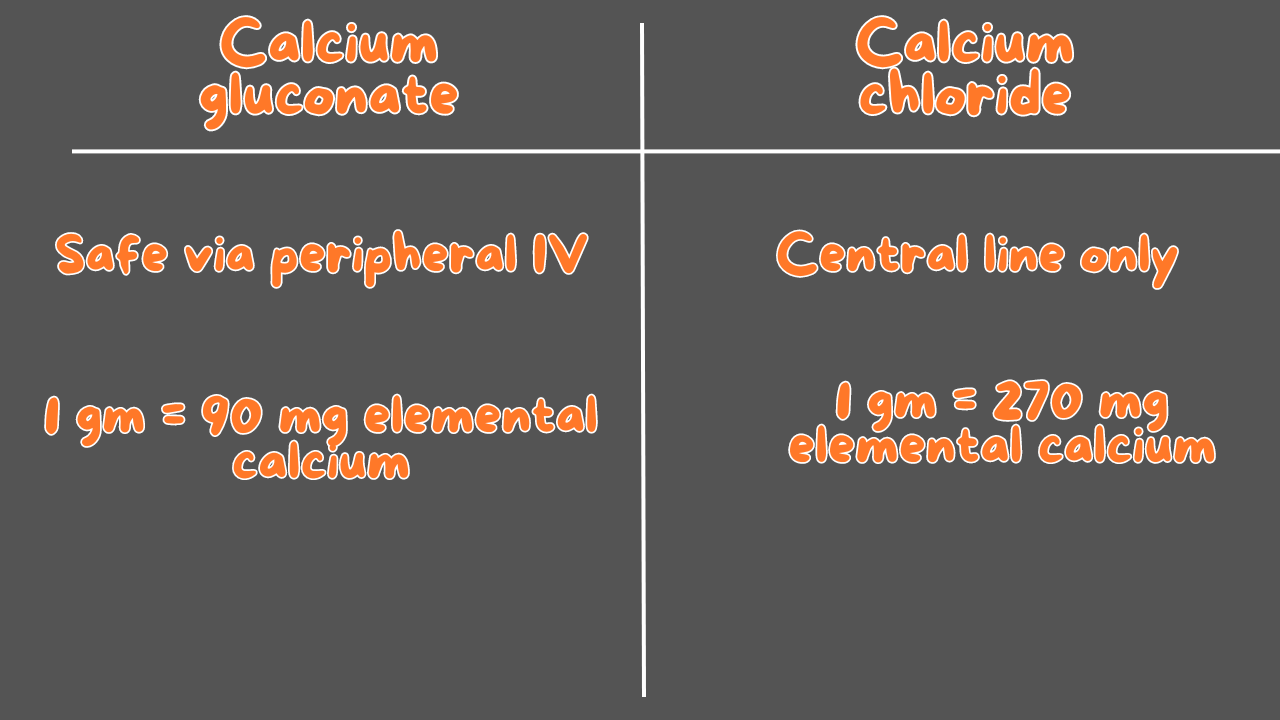
- Infuse 1-2 gm of Calcium gluconate or 0.5-1 gm of calcium chloride over 10 minutes. A second bolus may be given if symptoms persist
- Symptoms resolved or improved, follow that with slow calcium infusion:
- Calcium drip at 50 ml/hr.
- Repeated scheduled boluses (every 6-8 hours) infused over 1-2 hours.
- Calcium drip:
- Mix 11 gm of calcium gluconate (990 mg elemental calcium) in 1000 of 0.9 NS or D5W and infuse at 50 ml/hr.
- Or mix 3.67 gm of calcium chloride (999 mg of elemental calcium) in 1000 of 0.9 NS or D5W and infuse at 50 ml/hr.
- Start oral calcium as soon as possible.
- Start vitamine D if defecient.
- Discontinue IV calcium if: Symptoms resolved + oral calcium and vitamin D supplements started.
- Replace any magnesium deficiency as hypomagnesemia makes it difficult to treat hypocalcemia.
Outpatient/nonurgent treatment
- Start oral calcium to provide 1-2 gm of elemental calcium/day including dietary calcium.
- Start vitamin D if defecient.
Disease-specific treatments
- Acute hypoparathyroidism: Oral calcium and vitamin D (calcitriol) should be started together. This is in addition to the urgent treatment.
- CKD: Hyperphosphatemia is the problem here, high phosphorus level decreases free calcium level, Calcium acetate is the mainstay treatment as a phosphorus binder rather than a calcium supplement. Vitamin D (Calcitriol) should added if defecient.
- Vitamin D deficiency:
- Ergocalciferol (D2) and Cholecalciferol (D3) need to be metabolized to active forms by the kidney and liver.
- Calcitriol is an active form of vitamin D that bypasses the renal or hepatic metabolism with a quick onset of action, perfect in renal and hepatic impairments patients and when a fast response is required as in acute hypoparathyroidism.
Monitoring
- Watch the resolution of symptoms.
- Check calcium level in 12-24 hours.
- Discharge patient once symptoms resolved, calcium level is >= 8 mg/dl, and oral calcium and vitamin D started and tolerated.



10 Medications You Must Master Before Your ICU Rotation
Positive troponins! MI or not?
Comprehensive Guide to Antibiotic Spectrum: Gram-Positive, Gram-Negative, and Anaerobic Coverage
Comprehensive Guide to Antibiotic Spectrum: Gram-Positive, Gram-Negative, and Anaerobic Coverage
Comprehensive Guide to Antibiotic Spectrum: Gram-Positive, Gram-Negative, and Anaerobic Coverage
How to Measure Blood Pressure Correctly At Home
How to Measure Blood Pressure Correctly At Home
How to Measure Blood Pressure Correctly At Home