Quick intro
- All non-insulin diabetic medications are used exclusively for the treatment of type-2 diabetes (so far) and work by:
- Promoting insulin secretion as in sulfonylurea and Meglitinides.
- Improving sensitivity to insulin as in the thiazolidinediones (Thiazolidinediones).
- Decreasing hepatic glucose output as in Metformin.
- Delaying the delivery and absorption of carbohydrates from the gastrointestinal tract as in GLP-1, GIP receptor agonists, and DPP-4 inhibitors.
- Increasing urinary glucose excretion as in Sodium-glucose cotransporter-2 (SGL-2 inhibitors).
- Preventing intestinal glucose absorption as in alpha-glucosidase inhibitors (Acarbose)
Secretagogues vs nonsecretagogues
- Secretagogues promote insulin secretion from the pancreas regardless of food intake which means it may cause hypoglycemia. Sulfonylureas and Meglitinides are secretagogues.
- Non-secretagogues are medications that:
- Pancreas-independent ( Do not promote insulin secretion), Metformin, SGL-2 inhibitors, alpha-glucosidase inhibitors, and Thiazolidinediones belong to this type.
- Promote insulin secretion from the pancreas but only in response to food, Medications that potentiate incretin hormones function GLP-1 receptor agonists and DPP-4 inhibitors belong to this family
- Do not cause hypoglycemia unless combined with secretagogues or taken in conditions that precipitate hypoglycemia like critical illness, liver disease, adrenal insufficiency, NPO, ..etc.
Little about incretin hormones
Incretin hormones including GLP-1(Glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide), are secreted from the small intestine in response to eating! Incretin works on three sites:
- The stomach: slows down the emptying of food into the intestine.
- The brain: Suppresses our appetite so we stop eating.
- The pancreas: informs the pancreas about the incoming food to pump insulin into the blood in response to food, and reduces or inhibits glucagon production.
Incretin hormones coordinate pancreas insulin secretion with food intake and are only stimulated by nutrition coming through our gastrointestinal tract!
- GLP-1 receptor agonists, dual GLP-1 and GIP agonist, and DPP-4 inhibitors (indirectly) are two classes of medication that work to restore these effects. Will come to that soon!
Clinical benefits
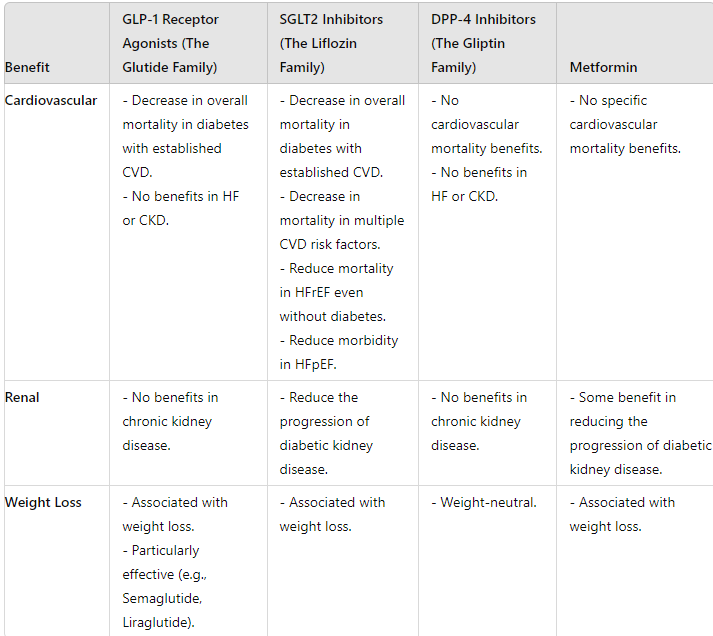
Clinical considerations
- All non-insulin diabetic medications should be suspended in:
- Patients with NPO status or poor oral intake.
- Critically ill patients.
- Patients with critical hyperglycemia where insulin should be used instead.
- The presence of specific drug contraindications.
- Non-secretagogues are preferred over secretagogues for type-2 diabetes treatment:
- Metformin remains the first line in type 2 diabetes treatment.
- SGL-2 inhibitors or GLP-1 receptor agonists or DPP-4 inhibitors come next
The patient’s underlying conditions will dictate which one to pick based on each class clinical benefits!
- Alpha-glucosidase inhibitors are not widely used because of relatively low efficacy, poor tolerance, and their cost.
- Thiazolidinediones use has dramatically decreased because of the association with HF and weight gain, if used, it’s usually pioglitazone.
- Secretagogues, especially sulfonylureas remain a good alternative when non-secretagogues can’t be used because of contraindications, affordability issues, or inadequate control with Non-secretagogues and insulin therapy isn’t preferred by the patient.
Metformin and glyburide are the only noninsulin antihyperglycemic drugs that are used in pregnancy.
Nonsecretagogues:
Metformin :
- Used in diabetes prevention in prediabetic patients, type 2 diabetes management, gestational diabetes if insulin can’t be used or along with insulin, and to induce ovulation in polycystic ovary syndrome.
- Gastrointestinal adverse reactions, including diarrhea, nausea, flatulence, dyspepsia, vomiting, and abdominal pain are the most commonly reported adverse reactions to metformin use, these symptoms are usually mild, transient, and reversible after dose reduction or discontinuation of the drug. Symptoms can be mitigated by starting at a low dose with slow-dose escalation as needed.
- Avoid Metformin in the presence of lactic acidosis or any condition that predisposes to lactic acidosis like:
- Volume depletion as in vomiting, diarrhea, bleeding, or sepsis.
- Decreased effective circulatory volume as in CHF exacerbations.
- Hypotension with or without a shock.
- In severe hepatic impairment, remember lactate gets metabolized in the liver.
- Contrast exposure within 48 hours (this may change in the future given that we have safer contrast agents nowadays)
- Hold Metformin if GFR < 30 or if any worsening in kidney function. Pay attention here we look at GFR not creatinine clearance.
- The long-term use of metformin may lead to B12 deficiency.
SGL-2 inhibitors (Sodium-glucose Cotransporter-2 Inhibitors)
- The Liflozin family: Empagliflozin, Dapagliflozin, and Canagliflozin.
- The only class that works in the kidney by promoting urinary glucose excretion.
- SGL-2 inhibitors have been associated with Normoglycemic DKA and Hypotension.
If a patient on the SGL-2 inhibitors presents with nausea, vomiting, and abdominal pain, check their AG and ketones even if they have BS < 250. Patients should be taken off SGL-2 inhibitors indefinitely if DKA confirmed.
- SGL-2 inhibitors are contraindicated to use in patients with a history of previous DKA.
- Because SGL-2 works on the kidney, we should avoid using them if eGFR < 30 mL/min/1.73 m2, unless they are used for DKD Then they can be used as long as GFR> 20.
GLP-1 receptor agonists
- The Glutide family: Dulaglutide, Exenatide {ER & IR}, Semaglutide, and Liraglutide, all are given SQ except semaglutide which can be given orally and SQ).
- Work by potentiating the effect of the incretin hormones (GLP-1).
- Terzipeptide is unique here because it is a dual GLP-1 and GIP receptor agonist.
- Nausea, vomiting, and diarrhea are prominent side effects of this class and can be severe and lead to severe cases of AKI requiring dialysis!
- Acute pancreatitis and acute cholecystitis have been associated with their use, So keep them in your differential when a patient presents with abdominal pain, nausea, vomiting, and diarrhea. They should be immediately suspended until proven otherwise!
- Contraindicated in patients with a personal or family history of Medullary thyroid cancer or patients with multiple endocrine neoplasia syndrome type 2 (MEN 2).
DPP-4 inhibitors (Dipeptidyl peptidase-4 inhibitors)
- The Gliptin family: Sitagliptin, saxagliptin, linagliptin, and alogliptin.
- They work by potentiating the effect of incretin hormones by preventing their degradation so they are kinda cousins of The Glutide family!
- They are taken orally compared to GLP-1 receptor agonists which are mainly taken SQ
- Similar to GLP-1 receptor agonists, they can also cause GI symptoms, acute pancreatitis, and acute cholecystitis.
- DPP-4 inhibitors are notorious for causing flu-like symptoms.
Alpha-glucosidase inhibitors
- The Bose family: Acarbose, miglitol, voglibose.
- Low efficacy and poor tolerance.
- They inhibit the upper gastrointestinal enzymes (alpha-glucosidases) that convert complex polysaccharide carbohydrates into monosaccharides thereby slowing the absorption of glucose and reducing postprandial blood glucose concentration.
- If hypoglycemia develops while on Alpha-glucosidase inhibitors, only pure glucose tablets should be used to reverse hypoglycemia, other forms of carbohydrates are less effective in raising blood sugar given how this class works!
The Thiazolidinediones (the glitazones family)
- They increase insulin sensitivity by acting on adipose, muscle, and, to a lesser extent, the liver to increase glucose utilization and decrease glucose production.
- Pioglitazone may still have some clinical uses, particularly in diabetic patients with biopsy-proven Non-alcoholic steatohepatitis (NASH), Pioglitazone improves fibrosis as well as inflammation and steatosis in such patients.
- The Thiazolidinediones should be avoided if:
- Heart failure or any evidence of fluid overload.
- History of fracture or at high risk for fracture (eg, postmenopausal women with low bone mass).
- Active liver disease (liver transaminases >2.5 times above the upper reference limit), unless NASH is known to be the underlying cause of the elevation.
- Active or history of bladder cancer.
- Pregnancy.
Secretagogues:
Sulphonylureas
- Glipizide, Gliclazide, Glimepiride, and Glyburide, Gliclazide isn’t available in the USA.
- Glipizide and Glimepiride are short-acting and safer to use in diabetics with CKD who are not dialysis-dependent yet.
- Glyburide is safe in pregnancy and can be used in gestational diabetes.
- Sulphonylureas have no cross-reactivity with other sulpha including sulfa antibiotics.
- Sulphonylureas remain good alternatives if other agents ( I mean Metformin, SGL-2 inhibitors, GLP-1 receptor agonists, DPP-4 inhibitors) can’t be used for any reason or are inadequate and the patient doesn’t prefer insulin-based therapy
Meglitinides (Repaglinide)
- Can be an option if a patient can’t use sulfonylureas because they are allergic to






The inpatient treatment of hypercalcemia
Hyperkalemia-induced EKG changes
The Proper Way to Replace Magnesium
Non-insulin diabetic medications
Chest Tubes & Pigtails: 5 Must-Know Tips for ICU Rotation
Mechanical Ventilation Made Simple: 9 Concepts Every Non-ICU Doc Should Know
NG Tube : 5 Things to know before your hospital rotations
Master ICU Vasopressor Management: 8 Shock Resuscitation Tips